From Researches Physiological and Pathological, 1824
Title: Blood Transfusion
Author: Geoffrey Keynes
Release date: January 11, 2021 [eBook #64268]
Most recently updated: October 18, 2024
Language: English
Credits: deaurider, John Campbell and the Online Distributed Proofreading Team at https://www.pgdp.net (This file was produced from images generously made available by The Internet Archive)
TRANSCRIBER’S NOTE
Footnote anchors are denoted by [number], and the footnotes have been placed at the end of the book.
Bibliography references are denoted by (number), and the list can be found near the end of the book.
Obvious typographical errors and punctuation errors have been corrected after careful comparison with other occurrences within the text and consultation of external sources. No other changes to the text have been made.
OXFORD MEDICAL PUBLICATIONS
BLOOD TRANSFUSION
BY
GEOFFREY KEYNES
M.A., M.D. CANTAB., F.R.C.S. ENG.
SECOND ASSISTANT, SURGICAL PROFESSORIAL UNIT
ST. BARTHOLOMEW’S HOSPITAL
LONDON
HENRY FROWDE AND HODDER & STOUGHTON
THE LANCET BUILDING
1 BEDFORD STREET, STRAND, W.C.2
First published in 1922
PRINTED IN GREAT BRITAIN
BY HAZELL, WATSON AND VINEY, LD.,
LONDON AND AYLESBURY.
[Pg v]
Blood transfusion is of rapidly growing importance in modern therapeutics, yet the subject has only been represented in the medical literature of this country hitherto by isolated communications concerning special points. The present work seeks to give a connected account of the whole subject and of the problems arising from it, together with practical instructions for performing transfusions by an efficient and simple method.
I am indebted for helpful criticisms and suggestions to Professor A. V. Hill, F.R.S., of Manchester University. Dr. J. H. Drysdale has kindly allowed me to use the records of three cases of pernicious anæmia treated in his wards at St. Bartholomew’s Hospital. Dr. Joekes has permitted me to refer to some of his own observations concerning abnormal serum reactions. Dr. R. M. Janes has given me some account of the important work recently done by Dr. Bruce Robertson and himself at the Hospital for Sick Children, Toronto.
The Bibliography at the end of the book makes no pretence of being absolutely complete. It is, however, more extensive than any that has yet been printed, and I believe that it contains references to nearly all the contributions of present importance published up to the date of going to press. Numbers referring to the Bibliography have been inserted in the text only where no name is given to the authority quoted.
Geoffrey Keynes.
86, Harley Street, W.1.
February 1922.
[vi]
[vii]
| CHAPTER I | |
| PAGE | |
| Historical Sketch | 1 |
| CHAPTER II | |
| Indications for Blood Transfusion: Hæmorrhage and Shock | 19 |
| CHAPTER III | |
| Indications for Blood Transfusion—continued: Hæmorrhagic Diseases—Blood Diseases—Toxæmias | 44 |
| CHAPTER IV | |
| Dangers of Blood Transfusion | 67 |
| CHAPTER V | |
| Physiology and Pathology of Blood Groups | 79 |
| CHAPTER VI | |
| The Choice of Blood Donor | 97 |
| CHAPTER VII | |
| The Methods of Blood Transfusion | 108 |
| Bibliography | 137 |
| Index | 159 |
[Pg 1]
BLOOD TRANSFUSION
From the earliest times the vital importance of blood to the human system has been fully appreciated. It has been supposed to carry in it some of the virtues, such as the youth and health, of its possessor, and it has therefore been commonly regarded as a sacrifice acceptable to the gods. References to blood in the Old Testament, in classical authors, and, it is stated, in the writings of the ancient Egyptians, refer rather to these mystical attributes than to any definite transference of it from the veins of one animal to those of another. One of the earliest references to actual transfusion of blood that has been noticed is to be found in a work by Libavius of Halle, published in 1615. The passage has been translated as follows:
“Let there be present a robust healthy youth full of lively blood. Let there come one exhausted in strength, weak, enervated, scarcely breathing. Let the master of the art have little tubes that can be adapted one to the other; then let him open an artery of the healthy one, insert the tube and secure it. Next let him incise the artery of the patient and put into it the feminine tube. Now let him adapt the two tubes to each other and the arterial blood of the healthy one, warm and full of spirit, will leap into the sick one, and immediately will bring him to the fountain of life, and will drive away all languor.”
It may be assumed, however, that this was only an idea, and had not yet been carried into practice. It was, indeed, unlikely that any attempt to perform blood transfusion[2] would be made until the conception of the circulation of the blood had been promulgated, and this in 1615 had not yet taken place.
William Harvey had been appointed physician to St. Bartholomew’s Hospital in 1609, and already in 1616 as Lumleian lecturer had stated his theory of the circulation, but not until its publication twelve years later could it be generally known. His treatise entitled Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus, which appeared in 1628, may therefore be regarded as the point from which blood transfusion first arose. It has often been stated in the literature of the subject that the first transfusion was performed in 1492, when the blood of three boys is supposed to have been transfused into the veins of the aged Pope Innocent VIII.[1] This, however, seems to have been a mis-statement of the facts. Actually a Jewish physician prepared a draught for the Pope from the blood of three boys, who were bled to death for the purpose.[2] The drinking of blood was not a new idea; this particular incident is of no special interest, and may now be allowed to sink into oblivion.
It is not until after the middle of the seventeenth century that authentic references to blood transfusion are to be found. The first is in the writings of Francesco Folli, a Florentine physician, who claims to have demonstrated the operation of transfusion of blood on August 13, 1654, to the Grand Duke Frederick II. There does not seem to be any confirmation of this in the writings of others. A few years later experimental work tending in the same direction was being done in England, and the inception of this was due to the ingenious Sir Christopher Wren, who in this connexion has not hitherto received the recognition that is his due. Dr. Wren, as he was designated at the time, was one of the most active members of the recently[3] formed Royal Society, and was responsible for many new experiments in several sciences. It is clear from references in the Philosophical Transactions that his first experiments were done in 1659, and the following statement is made by Dr. Thomas Sprat in his History of the Royal Society, published in 1667:
“He was the first author of the Noble Anatomical Experiment of Injecting Liquors into the Veins of Animals. An Experiment now vulgarly known; but long since exhibited to the Meetings at Oxford, and thence carried by some Germans, and published abroad. By this Operation divers Creatures were immediately purg’d, vomited, intoxicated, kill’d, or reviv’d according to the quality of the Liquor injected: Hence arose many new Experiments, and chiefly that of Transfusing Blood, which the Society has prosecuted in sundry Instances, that will probably end in extraordinary Success” (p. 317).
Sir Christopher Wren did not actually carry out any transfusion experiments on his own account. This was done by his friend, Richard Lower, well known for his work on the anatomy of the heart, who worked in the laboratory of Thomas Willis at Oxford. In these experiments, some account of which was published in 1666, he used a silver cannula for obtaining continuity between the artery of one animal and the vein of another. Lower must therefore receive the credit for having done the first transfusion actually performed in England. In the following year other experiments were done by Dr. Edmund King and Thomas Cox, both of whom recorded their experiences in the Philosophical Transactions.
Meanwhile Wren’s work had become known in other countries, and it is said that transfusion was performed in 1664 by Daniel of Leipsic, who thus anticipated the work of Lower. However this may be, the first transfusion done upon a human being was certainly carried out in France by Jean Denys of Montpellier, physician to Louis XIV. This is admitted in the Philosophical Transactions, but the[4] following statement in extenuation of English hesitancy is made:
“We readily grant, They were the first, we know off, that actually thus improved the Experiment; but then they must give us leave to inform them of this Truth, that the Philosophers in England had practised it long agoe upon Man, if they had not been so tender in hazarding the Life of Man (which they take so much pains for to preserve and relieve), nor so scrupulous to incurre the Penalties of the Law, which in England, is more strict and nice in case of this concernment, than those of many other Nations are.”
Dr. Edmund King further asserts that “We have been ready for this Experiment these six Months,” that is to say, since March, 1667. Moral precedence must, however, give way to the actual, and it is clear that Denys had snatched the laurels. A translation of a full and interesting account of his earlier experiment upon animals and his first two transfusions done upon men was published in the Philosophical Transactions for July 22, 1667. Of the first of these he wrote as follows:
“On the 15 of this Moneth, we hapned upon a Youth aged between 15 and 16 years, who had for above two moneths bin tormented with a contumacious and violent fever, which obliged his Physitians to bleed him 20 times, in order to asswage the excessive heat.
“Before this disease, he was not observed to be of a lumpish dull spirit, his memory was happy enough, and he seem’d chearful and nimble enough in body; but since the violence of his fever, his writ seem’d wholly sunk, his memory perfectly lost, and his body so heavy and drowsie that he was not fit for any thing. I beheld him fall asleep as he sate at dinner, as he was eating his Breakfast, and in all occurrences where men seem most unlikely to sleep. If he went to bed at nine of the clock in the Evening, he needed to be wakened several times before he could be got to rise by nine the next morning, and pass’d the rest of the day in an incredible stupidity.
[5]
“I attributed all these changes to the great evacuations of blood, the Physitians had been oblig’d to make for saving his life, and I perswaded myself that the little they had left him was extreamly incrustated [? incrassated] by the ardour of the fever.... Accordingly my conjecture was confirmed by our opening one of his Veins, for we beheld a blood so black and thick issue forth, that it could hardly form itself into a thread to fall into the porringer. We took about three ounces at five of the Clock in the morning, and at the same time we brought a Lamb, whose Carotis Artery we had prepar’d, out of which we immitted into the young man’s Vein, about three times as much of its Arterial blood as he had emitted into the Dish, and then having stopt the orifice of the Vein with a little bolster, as is usual in other phlebotomies, we caus’d him to lie down on his Bed, expecting the event; and as I askt him now and then how he found himself, he told me that during the operation he had felt a very great heat along his Arm, and since perceiv’d himself much eased of a pain in his side, which he had gotten the evening before by falling down a pair of staires of ten steps; about ten of the clock he was minded to rise, and being I observed him cheerful enough, I did not oppose it; and for the rest of the day, he spent it with much more liveliness than ordinary; eat his Meals very well, and shewed a clear and smiling countenance.... He grows fat visibly, and in brief, is a subject of amazement to all those that know him, and dwell with him.”
This boy had been transfused for therapeutic purposes; the second transfusion performed by Denys was done upon an older man “having no considerable indisposition,” and was purely experimental. About twenty ounces of lamb’s blood are stated to have been transfused, but the procedure was without any ill effect, and it may be doubted whether the man received as much as this.
In the succeeding number of the Philosophical Transactions, October 21, 1667, the remarks of another French[6] experimenter, Gaspar de Gurye, are quoted. These are of considerable interest, as they contain the first warning of the dangers attending the administration of incompatible blood. De Gurye affirms “that an expert Acquaintance of his, transfusing a great quantity of blood into several Doggs, observed alwayes, that the Receiving Doggs pissed Blood.”
Other cases were subsequently recorded by Denys. In one he claims to have cured a patient suffering from “an inveterate Phrenzy.” His account of it is too long to be quoted here in full, but it is of special interest in that it contains the first account of hæmolysis and the attendant symptoms in man which follow the transfusion of incompatible blood. The blood of a calf was used in this instance and on two occasions; at the first transfusion only a small amount was given, but at the second,
“the Patient must have received more than one whole pound. As this second Transfusion was larger, so were the effects of it quicker and more considerable. As soon as the blood began to enter into his veins, he felt the like heat along his Arm and under his Arm-pits which he had felt before. His pulse rose presently, and soon after we observed a plentiful sweat all over his face. His pulse varied extremely at this instant, and he complained of great pain in his Kidneys, and that he was not well in his stomack, and that he was ready to choak unless they gave him his liberty.
“Presently the Pipe was taken out that conveyed the blood into his veins, and whilst we were closing the wound, he vomited store of Bacon and Fat he had eaten half an hour before. He found himself urged to Urine, and asked to go to stooll. He was soon made to lie down, and after two good hours strainings to void divers liquors, which disturbed his stomack, he fell asleep about 10 a Clock, and slept all that night without awakening till next morning, was Thursday, about 8 a Clock. When he awakened, he shewed a surprising calmness, and a great presence of[7] mind, in expressing all the pains and a general lassitude he felt in all his limbs. He made a great glass full of Urine, of a colour as black, as if it had been mixed with the soot of Chimneys.”
The hæmoglobinuria, which was not at that time attributed to its true cause, cleared up in the course of a few days, and the patient appeared to be greatly benefited.
Although the first transfusion performed upon a human being was done in France, similar experiments were shortly afterwards carried out in England. The passage already quoted concerning the “sundry instances” mentioned in Sprat’s History of the Royal Society is amplified by the diarist, Samuel Pepys, who witnessed the experiments on at least one occasion. His first reference to the subject is under the date November 14, 1666:
“Here [at the Pope’s Head] Dr. Croone told me, that, at the meeting at Gresham College to-night, ... there was a pretty experiment of the blood of one dogg let out, till he died, into the body of another on one side, while all his own run out on the other side. The first died upon the place, and the other very well, and likely to do well. This did give occasion to many pretty wishes, as of the blood of a Quaker to be let into an Archbishop, and such like; but, as Dr. Croone says, may, if it takes, be of mighty use to man’s health, for the amending of bad blood by borrowing from a better body.” (Diary, ed. Wheatley, vi. p. 60.)
Two days later he reports:
“This noon I met with Mr. Hooke, and he tells me the dog which was filled with another dog’s blood, at the College the other day, is very well, and like to be so as ever, and doubts not its being found of great use to men,—and so do Dr. Whistler, who dined with us at the tavern.” (Ibid., p. 63.)
On November 28 there was further conversation at Gresham College to the same effect (ibid., p. 79). In the following year the experiments were taken a stage further,[8] and Pepys refers again to them under the date November 21, 1667:
“Among the rest they discourse of a man that is a little frantic, that hath been a kind of minister, Dr. Wilkins saying that he hath read for him in his church, that is poor and a debauched man, that the College have hired for 20s. to have some of the blood of a sheep let into his body; and it is to be done on Saturday next. They purpose to let in about twelve ounces; which they compute, is what will be let in in a minute’s time by a watch. They differ in the opinion they have of the effects of it; some think it may have a good effect upon him as a frantic man by cooling his blood, others that it will not have any effect at all. But the man is a healthy man, and by this means will be able to give an account what alteration, if any, he do find in himself, and so may be usefull.” (Diary, vii. p. 195.)
On November 29 Pepys dined at a house of entertainment, and enjoyed good company.
“But here, above all, I was pleased to see the person who had his blood taken out. He speaks well, and did this day give the Society a relation thereof in Latin, saying that he finds himself much better since, and as a new man, but he is cracked a little in his head, though he speaks very reasonably, and very well. He had but 20s. for his suffering it, and is to have the same again tried upon him: the first sound man that ever had it tried on him in England, and but one that we hear of in France, which was a porter hired by the virtuosos.”[3] (Ibid., p. 205.)
The subject of this experiment was Arthur Coga, an indigent Bachelor of Divinity of Cambridge, aged about thirty-two. It is recorded in the Philosophical Transactions that the experiment was performed by Richard Lower and Edmund King at Arundel House on November 23, 1667, in the presence of many spectators, including several physicians. Coga, when asked why he had not the blood of some other creature transfused into him, rather[9] than that of a sheep, replied: “Sanguis ovis symbolicam quandam facultatem habet cum sanguine Christi, quia Christus est agnus Dei.”[4] It was estimated that Coga received eight or nine ounces of blood, but he seems to have felt no effects, good or ill, and it is probable that he did not actually receive as much as this.
These beginnings in England and France led to the more frequent use of blood transfusion, but soon afterwards the operation fell into disrepute. Disasters followed the transfusions, and the practice also met with violent opposition on the ground that terrible results, such as the growth of horns, would follow the transfusion of an animal’s blood into a human being. In consequence of this they were actually forbidden in France by the Supreme Court until the Faculté of Paris should signify its approval, but the necessary permission was not given. The “extraordinary success” predicted by Sprat and the sanguine expectations of Pepys and his friends were destined not to be fulfilled until a later age.
For more than a hundred years the possibilities of blood transfusion were almost entirely neglected. There are some isolated references to it in medical writings towards the end of the eighteenth century, but of these it is only necessary to notice two. In 1792, at Eye in Suffolk, blood from two lambs was transfused by a Dr. Russell into a boy suffering from hydrophobia, and he claimed that the patient’s recovery was to be attributed to the treatment. Soon afterwards in 1796 Erasmus Darwin recommended transfusion for putrid fever, cancer of the œsophagus, and in other cases of impaired nutrition. He suggested that the blood should be transferred from donor to recipient through goose quills connected by a short length of chicken’s gut, which could be alternately allowed to fill from the donor and emptied by pressure into the patient. This operation he never actually performed.
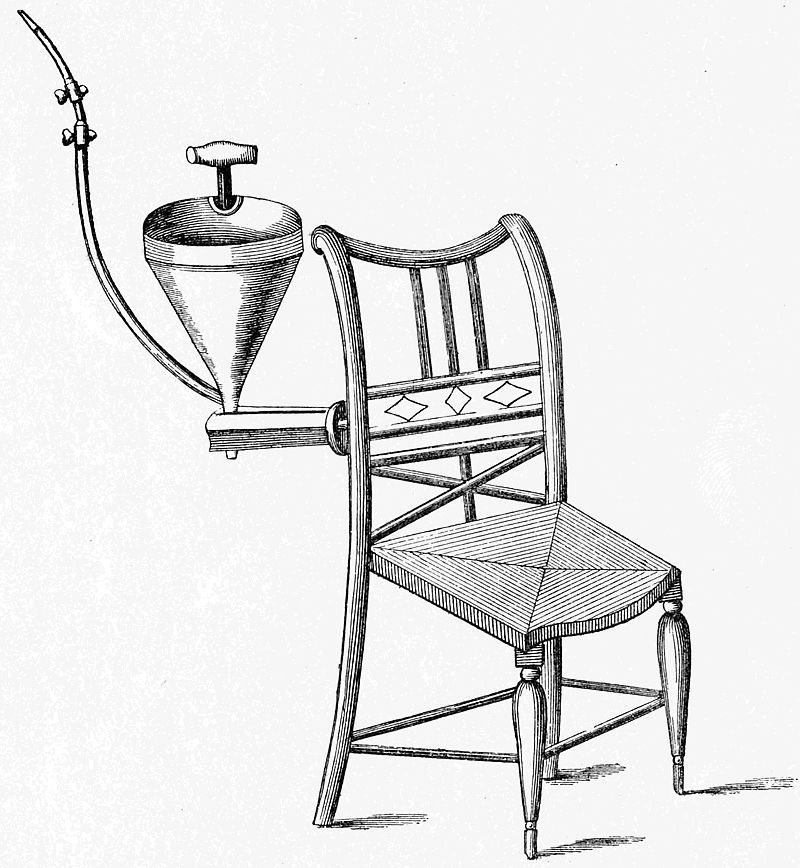
A more general interest in the subject was revived in[10] England by the work of James Blundell, lecturer on physiology and midwifery at St. Thomas’s and Guy’s Hospitals. He published in 1818 his earliest paper on experimental transfusion with a special form of syringe invented by himself. His first apparatus consisted of a funnel-shaped receptacle for the blood, connected by a two-way tap with a syringe from which the blood was injected through a tube and cannula into the recipient. His experiments were[11] performed upon dogs, and he began by drawing blood from the femoral artery and re-injecting it into the same animal through the femoral vein. He then conducted a long series of investigations into the properties of blood, the effects of its withdrawal, and the resuscitation of an exsanguinated animal. Soon he had opportunities of transfusing patients with human blood, and the results are recorded in his paper of 1824. His apparatus had by then been elaborated, and an engraving of his Impellor, as he termed it, is reproduced here. It consisted as before of a funnel-shaped receptacle for the blood, but the syringe was now incorporated in one side of the funnel, and contained a complicated system of spring valves, which caused the blood to travel along the delivery tube when the piston was pushed down. The Impellor was fixed to the back of a chair in order to give it stability.
All the patients transfused by Blundell were either exceedingly ill, or, judging from his description, already dead, so that his results, considered statistically, were not favourable! Nevertheless, he was not discouraged, and stated his “own persuasion to be that transfusion by the syringe is a very feasible and useful operation, and that, after undergoing the usual ordeal of neglect, opposition, and ridicule, it will, hereafter, be admitted into general practice. Whether mankind are to receive the first benefit of it, in this or any future age, from British surgery, or that of foreign countries, time, the discoverer of truth and falsehood, must determine.” Blundell’s work has been described in some detail because, after the experimental work of the seventeenth century, the year 1818 may be taken to mark the real beginning of the clinical application of blood transfusion.
The chief difficulty in the way of successful transfusion was, of course, the obstacle introduced by the coagulation of the blood. Bischoff in 1835 sought to overcome this by injecting defibrinated blood, and that solution of the difficulty was adopted by many operators, including Sir[12] Thomas Smith, who, in 1873, used defibrinated blood for transfusing a case of melæna neonatorum at St. Bartholomew’s Hospital. The apparatus on this occasion consisted of “a wire egg-beater, a hair sieve, a three-ounce glass aspirator syringe, a fine blunt-ended aspirator cannula, a short piece of india-rubber tubing with a brass nozzle at either end connecting the syringe with the cannula, a tall narrow vessel standing in warm water for defibrinating the blood, and a suitable vessel floated in warm water to contain the defibrinated blood.” Others, too numerous to be individually named, used the same method throughout the nineteenth century and during the first ten years of the twentieth. Even in 1914 a method of using defibrinated blood was described by Moss. An objection was raised in 1877 that it was dangerous to do this, owing to the excess of fibrin ferment introduced with blood thus treated, but this did not greatly discourage its use. Then, as now, one of the chief uses of blood transfusion was found to be in the practice of obstetrics. A series of 57 cases of this kind were reported by Martin of Berlin in 1859, 43 of these having been successful. A further series of cases was collected by Blasius in 1863. He was able to report that of 116 transfusions performed during the previous forty years, in 56 the results were satisfactory. These statistics did not indicate a remarkable degree of success. Fatalities due to the transfusion had occurred, attended by the symptoms which we have now learned to associate with incompatibility of the transfused blood. At that time, however, the deaths were believed to be due chiefly to the introduction of air bubbles into the circulation, although it had been shown experimentally by Blundell in 1818, and again by Oré in 1868, that small quantities, such as might be accidentally introduced during a transfusion, produced no ill effects. Some explanation, however, was required, and so air bubbles for a long time received the blame.
[13]
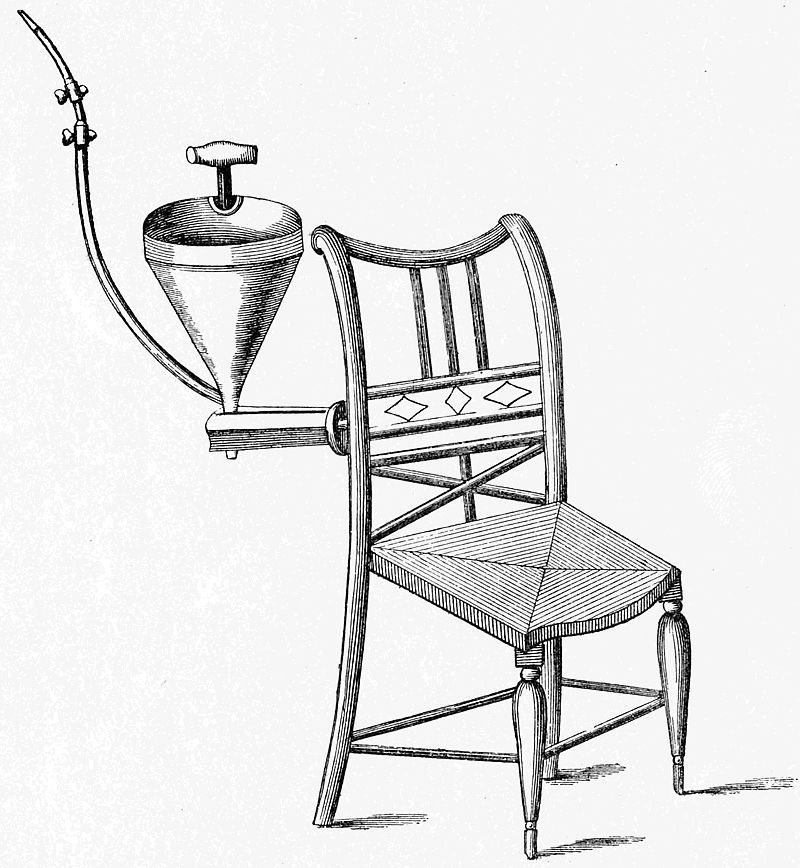
A is a metallic cup, of 6-oz. capacity, to receive the supply of blood. B an outer casing, which will hold 5 oz. of hot water, introduced through an aperture at C. D is a passage leading into an elastic barrel, composed of vulcanized india-rubber, E, of which the capacity is 1 oz. F′ the exit for the blood into the injection-pipe G. At D and F there are ball-valves, capable of closing the upper openings when thrown up against them, but leaving the lower openings always free. The blood, or other fluid, poured into the cup A, has free power to run unobstructed through D, E, F; a small plug H is therefore provided to close the lower aperture F when necessary. The tube G is of vulcanized india-rubber, and terminates in a metal tube O for insertion into the vein. This diagram is one-half the actual size of the instrument.
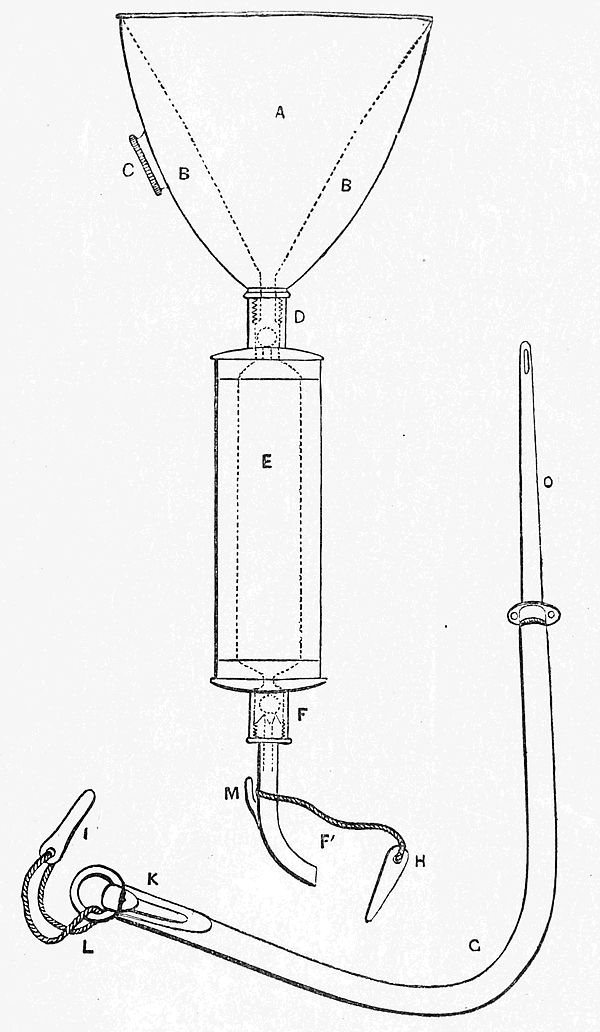
Although some of the early experiments on blood transfusion had been done in England, and although its revival [14]in the nineteenth century was initiated in England, yet it is to be noticed that most of the references to it up to 1874 are to be found in the works of Continental writers. Nevertheless, an important modification was introduced into the technique of the operation in 1857 by Higginson, who applied the principle of a rubber syringe with ball-valves for transferring the blood from the receptacle into which it was drawn, to the vein of the recipient. This apparatus is illustrated here, as it is of some interest in the history of medicine. Higginson’s syringe is now used for a different purpose, but it was successfully applied by its inventor in a series of seven cases which he duly reported. One patient whom he transfused was suffering from extreme weakness, which was attributed to the too protracted suckling of twins. He gave her about twelve ounces of blood from a healthy female servant, and a state of quietude followed her previous restlessness. A few minutes later the patient was seized with a rather severe rigor. It did not last long, but led to a state of reaction and excitement, in which she sang a hymn in a loud voice. The final result was good, and Higginson reports that in five of the seven cases some benefit was to be attributed to the transfusions. Later the same principle was used in America by Aveling and by Fryer about the year 1874, and subsequently it was in that country that nearly all the important advances in the science of blood transfusion were made.
In 1873 an inquiry was carried out by the Obstetrical Society of London into the merits of transfusion, the subject having been brought to the Society’s notice by a report of a case by Aveling, and an interesting summary of the evidence was prepared by Madge in 1874. The results do not seem to have been very encouraging, and transfusion was still regarded as a procedure that was only to be used as a last resource. Even at this date the blood of other animals was being used for transfusion, although the practice had been discredited by Panum in 1863 and by[15] others, and a series of cases was reported by Hasse in 1873, in which lamb’s blood was given for various conditions. Other cases were reported from Italy (3) and Russia (101). Sentiment, if not science, seems to have suggested that there was something repulsive in bringing a lamb into the sick chamber and mixing animal with human blood, but it was remarked in a discussion on the subject that “it was only taking lamb in another form.”
After 1875, however, there was a decline in the amount of attention given to transfusion which lasted for thirty years. This was probably due in part to the increasing number of fatalities which had followed the more general use of transfusion, but, as Peterson suggests, it was also to be accounted for by the increasing use of normal saline solution for intravenous injection in the treatment of hæmorrhage. There was also a period during which the use of milk was advocated for intravenous therapy (37, 279). Soon after the beginning of the twentieth century transfusion received a fresh impetus which has steadily gained force up to the present time. The free use of cannulæ and syringes had always been hampered by the coagulation of the blood, and it was clearly a great advance to be able to perform a direct transfusion without the intervention of any tube. This was made possible by great improvements in the surgery of the blood-vessels, which were due in the first place to the work of Murphy, published in 1897; they were carried still further by others, such as Carrel and Guthrie, and culminated in the work of Crile, who in 1907 put the technique of direct transfusion on a securer basis than it had ever been before. His method is briefly described in a later chapter of the present work. Meanwhile the chief factor responsible for previous fatalities was being eliminated. The presence of agglutinins and iso-agglutinins in the blood had been detected by Landsteiner and by Shattock in 1901; in 1907 the four blood groups into which human beings can be classified were determined by Jansky and the work was repeated by Moss in 1910.
[16]
Simplification of the group tests soon followed, as is described in another chapter. At the same time great improvements were made in the use of syringes, paraffined tubes, and in anastomosis of the blood-vessels. In this connexion one of the most notable contributions was made by Curtis and David, who in 1911 introduced the use of syringe transfusion through a two-armed tube coated on the inside with paraffin. In 1913 indirect transfusion by means of the paraffined vessel was introduced by Kimpton and Brown, and it was now evident that blood transfusion was shortly to become a method of treatment which would be without any very difficult technique, and could therefore be more extensively applied.
The final advance was made in 1914, when the use of sodium citrate as an anticoagulant was made possible by the work of Lewisohn in America, of Hustin in Belgium, and of several others, who all arrived independently, but almost simultaneously, at the same conclusion. The use of an anticoagulant was no new idea. In 1858 the use of small quantities of ammonia had been suggested by B. W. Richardson in the Guy’s Hospital Reports, and in 1869 sodium phosphate was used in four obstetrical cases by Braxton Hicks, who found that the process was greatly facilitated thereby; but neither of these methods came into general use. It had long been known that hirudin or leech extract, and the salts of oxalic acid or of citric acid, could be used as anticoagulants outside the body, but their supposed toxicity had prevented their being used for transfusion. The proof that sodium citrate was both efficient for this purpose and non-toxic in a dilution that was still effective at once raised blood transfusion to a wider sphere of usefulness than had been possible before. The first transfusion of citrated blood was performed by Professor L. Agote of Buenos Aires, on November 14, 1914, a date which is therefore of the greatest importance in the history of blood transfusion. A method had at last been discovered which approached the ideal, since it united the[17] four cardinal virtues of simplicity, certainty, safety, and efficiency.
This great stride forward in the technique of blood transfusion coincided so nearly with the beginning of the war that it seemed almost as if foreknowledge of the necessity for it in treating war wounds had stimulated research. Yet during the first two years of the war almost nothing was known in the British Army of its possibilities. I have no evidence that the French or German army doctors were any better informed than ourselves. Some attempt was made in 1916 to introduce the use of direct transfusion through cannulæ, but the technique was too difficult and uncertain for the stress of war conditions. It was not until 1917, when the British Army Medical Corps was being steadily reinforced with officers from the United States of America, that knowledge of blood transfusion began to be spread through the Armies. A conspicuous part was borne by Oswald Robertson in introducing the use of the citrate method, and to him a very large number of men indirectly owe their lives. In some armies the paraffined vessel of Kimpton and Brown remained the favourite method, but to me the citrate method seemed the more suitable, because of the certainty with which success could be attained, and the same view was taken by many others. At the same time the investigators appointed by the Medical Research Committee attempted to elucidate the problems connected with hæmorrhage and wound shock, and their results, as will be seen, served to confirm the estimate already being formed of the value of blood transfusion.
In this way a large number of operators in this country became familiar with the various methods, and transfusion has in consequence been used increasingly in civilian practice since the war. It is undoubtedly destined to figure still more largely in the therapeutics of the future. Meanwhile the public mind is becoming gradually more used to the idea, and the time is past when every transfusion[18] is deemed worthy of a sensational headline in a newspaper. Nevertheless, at the end of the year 1920 the following advertisement appeared in the personal columns of The Times:
“Will any Doctor who knows method of treating cancer by transfusion of child’s blood kindly write Box —.”
So the wheel is come full circle, and the shade of Pope Innocent VIII may well chuckle as he notes the small advance in popular knowledge since the fifteenth century.
[19]
The indications for blood transfusion are gradually becoming more numerous as experience of its effects accumulates, and there can be no doubt that the value of transfusion as a therapeutic measure is destined to become much more generally recognized than it is at the present time. Lack of knowledge, together with an exaggerated idea of the difficulties of the process, is the chief obstacle to its more extended use. Time and the education of the rising generation will provide the remedy for this.
The conditions for which blood transfusion may be used fall into four well-defined groups. On the one hand are those characterized by an acute anæmia, which demand the performance of a blood transfusion as an emergency or life-saving operation; on the other hand are those in which the anæmia is of slow onset, and is to be combated by a single transfusion to tide the patient over an operation or a critical period or by repeated transfusions in the hope of prolonging the patient’s life if not of obtaining a cure. A third group includes the hæmorrhagic diseases in which the transfusion is administered not only to replace blood which has been lost, but also to bring about cessation of the hæmorrhage. A fourth group includes cases of general toxæmia, whether chemical or bacterial, in which the new blood is given partly on account of its therapeutic properties, partly in order to dilute the circulating toxins or to supply healthy red blood cells to carry on the oxygenation of the tissues.
For the first and third of these groups blood transfusion[20] is now very firmly established as a method of treatment which is of extraordinary value. For the second group it may be regarded as a palliative to be given with circumspection. For the fourth group administration of blood is still in the experimental stage.
In the present work each condition will be taken in turn and, as far as possible, separately, though at the outset it has been found undesirable to dissociate the two conditions, hæmorrhage and shock. The present position of blood transfusion in relation to each condition will be discussed; its limitations and the precautions to be observed will be described.
Blood transfusion is pre-eminently the best form of treatment that is known for the condition of acute anæmia following hæmorrhage to whatever cause it may be due. Its good effects were seen by a number of operators in many hundreds of exsanguinated patients during the latter part of the war, and its value was then established upon a secure foundation. It was unusual during the war to meet with patients who were in danger of their lives from loss of blood alone without the additional factor of traumatic shock, but such cases did occur, and they are also to be met with in civil practice, as, for instance, in attempted suicide by throat cutting, in gastric ulcer with severe hæmatemesis, and in secondary hæmorrhage after operation. The more typical condition following war wounds, hæmorrhage with shock, will be faithfully reproduced in the victims of train or street accidents, in patients who have undergone certain severe operations, and in women suffering from post-partum hæmorrhage or a ruptured ectopic gestation.
The signs and symptoms of acute anæmia will be familiar to most readers. It is characterized by a peculiar greyness of the skin, by extreme pallor of the mucous membranes, by a cold perspiration, by a thready and rapid pulse which[21] may exceed 140 beats to the minute, and by extreme restlessness. The “amaurosis” of the text-books is seldom met with, but in the last stages the patient becomes semi-unconscious, the restlessness tends to disappear, the muscles relax, and the respiration takes on a peculiar sighing character, which is described as “air hunger,” and probably indicates exhaustion of the respiratory centre. Meanwhile, if instruments are at hand, additional signs may be recognized. The most important of these is a fall in blood pressure. It has been stated that a systolic pressure below 70 mm. of mercury is scarcely compatible with life, but this is not in accordance with experience. It was common during the war to meet with blood pressures below 45 mm., so low in fact that they could not be measured with the ordinary apparatus that was available, but many patients whose lives had reached even so low an ebb as this were quickly restored by the administration of blood, provided that the exsanguinated state had not lasted for too long a time. If the medullary centres are damaged beyond recovery by inadequate oxygenation lasting for several hours, then no treatment is of any avail. But provided that it be given before this length of time has elapsed, a blood transfusion may succeed in saving life at any stage of the condition. Its efficacy is indeed only limited by the actual cessation of the patient’s heart beats. I have successfully treated a patient who before transfusion could only be described as moribund. He was almost unconscious, absolutely blanched, and his radial pulse imperceptible; his jaw was relaxed and his breathing had become a series of fish-like gasps, such as are only associated with imminent dissolution. His heart would certainly have ceased beating within a few minutes, yet his condition improved so rapidly after transfusion that an hour later it was possible, with the help of a second transfusion, to amputate his leg above the knee. This patient ultimately recovered, having been as near death as it is possible to be and yet remain alive.
[22]
The results of a blood transfusion upon a patient suffering from acute anæmia are, indeed, amongst the most dramatic effects to be obtained in the whole range of surgery. Within a few minutes of its commencement the whole aspect of the patient alters. His respiration becomes deep and regular, his restlessness disappears, colour returns to his face, his pulse rate falls, and he begins to take an intelligent interest in his surroundings. These changes taking place within a period of fifteen minutes may well strike an onlooker as little short of miraculous. Shortly afterwards the patient may fall into a natural sleep, a sure sign that the normal circulation has been restored to the exhausted central nervous system.
In considering how much blood should ordinarily be given in the treatment of acute anæmia, experience is a safer guide than any theoretical considerations. Nevertheless, it is worth while to inquire briefly into the experimental and theoretical basis upon which the treatment of acute anæmia rests. It is difficult to estimate accurately the total quantity of blood in the body of an adult, but it has been variously stated by physiologists to be from a twentieth to a tenth part of the body weight, or, in liquid measure, from 3 to 6 litres (approximately 5 to 10 pints). This has been estimated in several ways, the results of which show some discrepancy. A figure approaching the higher one was obtained long ago by the direct method of washing out the blood from the bodies of executed criminals. Recently it has been claimed by Haldane that these determinations were inaccurate; by means of his carbon monoxide method, with the details of which we are not concerned here, he has estimated that the blood volume is but one-twentieth of the body weight, or in very stout persons is even as low as one-thirtieth. Still more recently Haldane’s estimation has been challenged in its turn by observers who have injected a dye into the circulation and have then determined its degree of concentration in the blood by means of colorimetric[23] comparisons. It is evident that if the dilution which occurs when a known quantity of dye is injected can be accurately estimated, then the total volume of circulating fluid can be calculated. This method could not be used until a non-toxic, non-diffusable dye had been discovered, but it was found in 1915 that “vital red” fulfilled these requirements (143). The results obtained in this way show that those originally given by the direct method were substantially correct. The blood volume was found to vary from 1/13 to 1/10·5 of the body weight; on the average it amounted to 5,350 cc., or 85 cc. per kilogram of body weight. These observations have been in their turn criticized (114), but only to the extent of reducing the amount by 1/10. It may therefore be assumed that, according to the most recent work, the blood volume is from 5 to 6 litres, or, approximately, 8 to 10 pints.
It is a still more difficult matter for obvious reasons to estimate how much blood a man can lose and yet remain alive. This will depend partly on the power of physiological accommodation possessed by the individual in his vaso-motor system and tissue fluids and partly on the rapidity with which the bleeding takes place. Clinical observations have shown that after a moderate hæmorrhage, such as the withdrawal of 800 cc. of blood from a donor, the blood volume may be restored to normal within an hour. If, on the other hand, the hæmorrhage is excessive, a condition results in which the normal process of rapid restoration of volume fails, and the circulation remains in a dangerously depleted condition. The heart attempts to keep the blood pressure at an adequate level by an increase in its rate, but it is in effect attempting to circulate a small volume of fluid in a vascular system which has become too big for it. Imperfect oxygenation of the medullary and cerebral centres with exhaustion of the heart results, and this is accompanied by all the symptoms of anæmia which have been already described.
If the initial hæmorrhage be very rapid, death may result[24] almost at once, since the physiological processes may have no time to act. On the other hand, a rapid hæmorrhage may under certain circumstances save the patient’s life, for the immediate syncope which results produces so great a fall in the blood pressure that hæmorrhage almost ceases and a clot may form in the lumen of the divided vessel. If the hæmorrhage be more gradual, the physiological compensation may at first be adequate to maintain the blood volume, but finally a point is reached at which this process fails and the patient then passes into the condition of acute anæmia.
The actual amount of blood therefore that must be lost to be fatal will vary according to circumstances. Experience shows that hæmorrhage may take place into the peritoneal or pleural cavities to the extent of two litres or even more, and it may be stated as a rough guess that 2·5 litres, that is to say, even as much as almost half the total blood volume, may be lost without immediate death resulting. This degree of depletion could not, however, be endured for long. A series of clinical observations made by Keith by the vital-red method upon the blood volume in soldiers suffering from the combined effects of hæmorrhage and wound shock showed that in the most serious cases the volume was below 65 per cent. of the normal, frequently even between 50 and 60 per cent. Serious symptoms followed a reduction to between 65 and 75 per cent. In patients without distressing symptoms the volume was never below 75 per cent. of the normal. There is direct evidence, therefore, that those patients who are most in need of treatment, such as a transfusion of blood, will probably have lost from 25 to 50 per cent. of their blood volume, that is to say, 1·5 to 3 litres in amount, and will need from 750 cc. to 1·5 litres to restore them to, or near to, the 75 per cent. level at which the compensatory processes can begin to regain their power.
It is thus possible to arrive at a theoretical basis on which an idea can be formed of the amount of blood that should[25] be given in acute anæmia. Practical experience is in agreement with the theory, and it will now be easier to understand how it is that in treating acute anæmia no attempt need be made to replace the whole amount of blood that has been lost, or indeed anything approaching it. In an extreme case 2 to 3 litres of blood will have been lost and 1 litre or more will be needed to restore the blood volume to approximately 75 per cent. of the normal. A case of this sort, however, is fortunately not often to be met. One has already been described on page 21; this patient received altogether nearly 1,600 cc. of blood in two transfusions, and 1,000 cc. of normal saline were given in addition.
In most cases of severe hæmorrhage the patient has probably not lost more than 1,400 to 1,800 cc. of blood, and 600 to 800 cc. will be enough to restore the balance of the circulation. This is in practice the amount of blood that is commonly administered, and it is well within the limits of what a single blood donor can afford to lose. If a more definite standard be required, it may be laid down that in a single transfusion for acute anæmia 750 cc. of blood should be given. If, in an exceptional case, more than this is needed, a second transfusion should be performed with a similar amount taken from another donor. Sometimes it may happen that a patient already in extremis from loss of blood, needs a severe operation; in such a case a second transfusion may be given with great advantage at the conclusion of the operation. The first transfusion will restore the patient sufficiently to render the performance of an operation possible; the second will combat the additional shock and hæmorrhage which it has caused.
It has already been stated that it was uncommon during the war to meet with patients who were suffering from anæmia uncomplicated by traumatic shock. It was in fact the condition of shock which tended to dominate the clinical picture, and it was towards the elucidation of the[26] facts concerning shock, its causation, prevention, and treatment, that the investigations co-ordinated by the Medical Research Committee were mainly directed. These investigations were carried out both in the laboratory and in the military hospitals, and considerable additions were made to the knowledge of the condition. It is necessary to give some account of the conclusions which were reached in order that the rôle of blood transfusion in the treatment of shock may be fully understood.
Hæmorrhage and shock cannot be dissociated, and this is not only because they so frequently occur together in the same patient, but also because the manifestations of the two conditions are essentially the same. In shock, as in hæmorrhage, are found the same pallor of the face and mucous membranes, the same fall of blood pressure and rapid pulse, the same perspiration, restlessness, and shallow respiration. The symptoms following a severe hæmorrhage have sometimes been referred to as constituting a “shock-like condition.” As will be seen, however, it is more accurate to describe the symptoms of shock as closely resembling those of hæmorrhage, and to regard both conditions as a manifestation of deficient fluid content in the circulation.
Numerous theories have been advanced to account for the symptoms seen in shock. Until recent years it was customary to suppose the vaso-motor centres had failed, being overcome by exhaustion consequent upon excessive stimulation by a greatly increased number of afferent impulses from the periphery of the body. It was suggested that as a result there was a general dilatation of the vascular system, especially in the abdominal veins, and therefore a general impairment of the circulation. Various hypotheses were, in addition, formulated, to account for the vaso-motor failure. These included the ideas of deficient carbon dioxide in the blood, exhaustion of the adrenal secretion, and exhaustion of nerve-cells in the higher centres. All these theories found their supporters[27] and much experimental evidence was brought forward, but none was susceptible of final proof. The whole theory of vaso-dilatation and the idea that the patient “bleeds into his own abdominal veins” were eventually disposed of by observation of the clinical facts. Many extensive abdominal operations have been performed upon shocked patients, but the accumulation of blood in the splanchnic area has never been demonstrated. It has, on the other hand, been found that in the limbs the arteries and arterioles are strongly contracted. It is also by no means unusual to meet with the condition known as venospasm; the veins are collapsed and their walls contracted, so that it becomes necessary to use a considerable positive pressure before any fluid can be induced to flow into them. It has, in addition, been shown that the vaso-motor system is still active, and the heart, although beating rapidly, still responds to reflex stimulation and to increase of intracranial tension.
It becomes necessary, therefore, to find some other explanation of the low blood pressure which is the essential feature of shock. Of especial value in this connexion are the investigations by Keith, already mentioned, into the changes in blood volume found in soldiers suffering from shock and hæmorrhage. In very few of these cases were the symptoms due to shock alone, but usually the loss of blood volume was much greater than could be accounted for by the amount of hæmorrhage which had taken place. Here, therefore, was evidence strongly suggesting that the symptoms of shock are due to actual loss of circulating fluid, and the problem now resolved itself into a search for this fluid which has ceased to be part of the effective blood volume. Enough has already been said to show that there is no evidence that the larger vessels, whether arteries or veins, are acting as reservoirs in which the blood is stagnating. It therefore only remains to consider whether the capillary system is capable, under abnormal conditions, of holding so large a proportion of the blood as[28] has been shown by Keith to have left the circulation. For a discussion of this problem the reader may be referred to W. B. Cannon’s summary of the arguments (45), from which it becomes clear that the capillary system may be regarded as a potential reservoir large enough to contain the lost blood in shock. The question is, however, further complicated by the fact that the capillary blood in shock differs from the circulating blood in containing an abnormal concentration of corpuscles. Extensive observations made on wounded soldiers have shown that the number of red blood cells may rise even to 8,000,000 per cmm. in the capillary blood, while the number in the venous blood remains at 5,500,000 or less. This concentration of the red cells is gradual and progressive, and will by itself account for a large part of the loss of volume, since normally the bulk of the blood is made up of corpuscles and plasma in approximately equal parts. The stagnation is, moreover, accentuated by the increased viscosity of the blood resulting from the concentration, and by the chilling of the surface of the body, which is always a feature of the state of shock. A vicious circle is thus established, and the symptoms of shock become severe as the capillary stagnation becomes more pronounced.
A second factor which may also play its part in the loss of blood volume in the general circulation is the exudation of some of the plasma into the surrounding tissue spaces. As the stagnation increases, oxygenation decreases, and the walls and the capillaries become more permeable, so that some fluid is probably lost in this way. This permeability may also be accentuated by the increased hydrogen-ion concentration in the blood, which often accompanies shock, but it seems to be clear that this is a secondary phenomenon resulting from imperfect oxygenation in the tissues, and it will therefore not be regarded as one of the factors responsible for shock. Further fluid is lost by the copious perspiration commonly seen in shock. There seems, therefore, to be a conspiracy between a whole set of[29] different factors all tending to deprive the patient of his circulating fluid. The net result is a condition so closely resembling hæmorrhage that it may be impossible to distinguish the two, this difficulty being increased by the fact that they so often occur together.
In the foregoing account of the production of shock the fate of the lost blood has been discussed, but nothing has been said of the factors initiating the capillary stagnation. This is a subject which is of great interest and some obscurity, and is of evident importance in considering how shock may be avoided. The present treatise, however, is primarily concerned with the treatment of shock when already established, and it is therefore not proposed to follow out the other question in detail. An injury may be followed immediately by a condition of “primary wound shock,” in which the patient becomes suddenly pale and pulseless. This is a physiological reaction, which may be transient, and it is to be distinguished from the much more serious condition of “secondary wound shock” which appears some time later. It is this secondary shock alone which has been under consideration in the preceding pages. The chief importance of the primary shock lies in the fact that it may initiate the conditions which predispose to secondary shock, so that under certain circumstances the one may become merged in the other. These predisposing conditions are increased evaporation from the skin, a general fall in the temperature of the body, mental anxiety, and the continued stimulation of the higher centres by afferent impulses as is manifested by pain. The condition of secondary wound shock was shown in a striking degree, during the earlier years of the war, by the men suffering from fracture of the femur. In the later part of the war warmth was supplied more systematically than before to the seriously wounded, and all fractured femurs were treated at an early stage with Thomas’s splints. Two of the factors predisposing to shock, namely cold and pain, were in this way to some[30] extent eliminated, and it was very striking how much better than before was the general condition of the patients on arrival at the hospitals.
Nevertheless, the elimination of these factors, which is a simpler matter in civil life than it was under conditions of war, will not avert all shock in a large proportion of cases. It is necessary, therefore, to find some additional factor which will initiate shock in addition to the predisposing causes. It is thought that this may have been identified in a substance of obscure nature which is derived from the damaged tissues themselves, and which, circulating in the blood, is able directly to affect the capillary system. Just as the shock following severe burns is believed to be due to the circulation of a toxic substance formed by the burning of the skin and other tissues, so the shock following severe trauma is believed to be of toxic origin, the toxin being derived from damaged tissues, muscle being particularly active in this respect. The condition may, therefore, be one of “traumatic toxæmia,” in which there is a general loss of capillary tone throughout the body, so that “the blood percolates into the network of channels as into a sponge.” The circulating blood is thus rapidly depleted, and the symptoms of shock become established. The investigation of this source of shock was carried out chiefly by Dale, Bayliss and Cannon (65), who were able to reproduce the condition of shock in animals by the injection into their circulation of a substance obtained from damaged muscles. To this substance the name histamine was given. It would be a mistake, however, to suppose that because a substance producing shock experimentally has been obtained from muscles, that therefore this is the identical substance which is responsible for every case of traumatic toxæmia. Extreme shock may be produced when but little damage has been done to muscles. Probably damage to any tissue of the body if extensive enough will produce a substance or substances which will give rise to the symptoms, and it may be a long[31] time before these are isolated and identified. That the last word on the production of shock is still far from being uttered is shown by the fact that profound shock may be induced without doing any appreciable damage to tissue, namely, by handling and exposing the abdominal viscera.
It may be this traumatic toxæmia which will account for many cases of post-operative shock, but it has been shown that some anæsthetics, such as chloroform or ether, will of themselves greatly accentuate shock initiated by other causes.
It has already been mentioned that the increased hydrogen-ion concentration in the blood, which results from imperfect oxygenation in the tissues, is not itself a cause of shock, but it will aggravate shock due to other factors. A discussion of this will be found in the paper by W. B. Cannon already referred to.
The present state of knowledge concerning the causation of shock having been thus briefly reviewed, the question of the treatment of the condition may be discussed. In this connexion the value of blood transfusion will be considered. It will have become clear that essentially the condition to be combated in treating shock is one of lowered blood pressure following upon a diminution of the volume of blood in the circulation. All the factors which have been mentioned in considering the causation of shock must be combated. Warmth must be supplied, morphia administered, fractures efficiently immobilized, damaged tissues excised: but clearly all these measures are prophylactic rather than curative. None of them will remove a state of profound shock once established, for they will not of themselves restore the blood volume depleted by capillary stasis. It is necessary, therefore, to attack this condition directly. It may with justice be compared to a state of acute anæmia following hæmorrhage, but with this difference, that the blood is still present in the body and will return to the circulation when the capillary stasis has been abolished and the circulating balance has been[32] restored. The possibility of recovery from shock depends upon how long the condition has existed. After a certain time the toxæmia, whether the primary traumatic toxæmia or the secondary increase in hydrogen-ion concentration, appears to have a damaging effect upon the capillary walls, so that an increased loss of fluid takes place into the tissues and this cannot be remedied. It is essential, therefore, to use the means which will most rapidly restore the circulation and bring about a rise in blood pressure which will be permanent. It is reasonable to infer that the most hopeful means of bringing this about is by a blood transfusion, which will actually replace the blood temporarily lost. This is the physiological remedy, and its value has been proved by the results obtained in many cases of my own as well as in those recorded by others. The efficiency of the treatment is accentuated by the fact that so large a proportion of cases of shock are associated with, and aggravated by, some degree of hæmorrhage. Apart from this, Keith’s observations have shown that the diminution of blood volume in shock is comparable with that which attends severe hæmorrhage. The state of shock in fact so closely resembles hæmorrhage that most of the same remarks concerning blood volume and the amounts that should be given by transfusion may be applied, and it is unnecessary to repeat them here. It must be remembered, however, that in pure shock the amount of hæmoglobin in the body is not reduced though there is less in the circulation. It is restored to the circulation when the capillary stagnation is overcome. This will be referred to again later on.
During the war the value of blood transfusion in shock was amply demonstrated. In civilian practice I have found it to be of value when given after operations such as removal of the rectum, whether by the perineal or abdomino-perineal route, amputation of the leg through the hip joint, or removal of a sarcoma from the nasopharynx. Transfusion should be given towards the close of the operation[33] before the evidences of shock have reached their maximum. The depletion of the blood volume is then actually remedied as it takes place, and transfusion becomes almost as much a prophylactic measure as warmth and the administration of morphia.
It is probable that the mortality following very severe operations such as those mentioned above would be considerably reduced if blood transfusion were to be given as a routine measure. Reference has already been made to the bad effect of the ordinary anæsthetics, and the best effects are obtained by a blood transfusion in conjunction with gas and oxygen or with spinal anæsthesia. It is necessary, however, to draw attention to the fact that a blood transfusion if given to a patient under the influence of a spinal anæsthetic must not be performed until the operation is very nearly completed, for it will very often produce a much more rapid return of sensation than would otherwise occur.
In advocating the use of blood transfusion to combat the effects of shock and hæmorrhage, it would be misleading to imply that this is necessarily the only treatment that is available. Something must be said of the substitutes for blood that have been used, and in particular the value of gum acacia must be considered. In the days before the war it was customary to treat post-operative shock or hæmorrhage with large quantities of normal salt solution given intravenously or subcutaneously. During the earlier part of the war also this was used, and there can be no doubt that for the less severe cases this treatment is often beneficial. Occasionally even the lives of patients who were desperately ill have been saved by it; I have seen a saline infusion cause the recovery of a man who had a dozen perforations of the small intestine and who had, in addition, lost several pints of blood intraperitoneally from a wound of a large mesenteric vessel. Such cases are, however, exceptional. In the presence of severe shock or hæmorrhage a saline infusion may cause an immediate rise in[34] blood pressure, but the fluid exudes so rapidly into the tissues that the effect is usually very transient. This fact is universally admitted to be true and need not be further emphasized. Saline solution administered by the rectum is likely to have a more lasting effect, but the process of absorption is slow, and the patient may be dead before it has had time to act. The same applies to water given by the mouth. A patient suffering from severe shock is unable to tolerate more than a very small quantity of fluid in his stomach without vomiting. Some success was attained by Oswald Robertson in treating cases of hæmorrhage by the method of “forced fluids,” large quantities being given by the mouth and by the rectum (245). In many serious cases, however, this treatment is inapplicable, and it is clear that transfusion is more rapid and more certain in its effect. Isotonic saline having been found ineffectual, it was suggested that a hypertonic solution (2 per cent. sodium chloride) might be of more value. This was tested clinically and in the laboratory, and was found to have no advantage over the isotonic solution (11).
When the association of increased hydrogen-ion concentration with shock was demonstrated, it was at first supposed to be one of the factors producing the condition. It was therefore natural that the effect of a solution of sodium bicarbonate (4 per cent.) should be tried. The effect upon certain cases suffering from extreme “acidosis” and air hunger was very striking, but in general the alkaline solution was no more effective than the ordinary isotonic saline. I soon abandoned its use for intravenous infusion, but it was of service in serious cases when given by the rectum.
During the war the necessity for the conservation of time—and of blood—was evident. The search for a satisfactory substitute for blood was therefore prosecuted with great energy, most of the research being done by, or under the direction of, Professor W. M. Bayliss. The[35] object of the research was to discover a non-toxic solution which possessed the same “viscosity” as the blood, and the same osmotic pressure due to contained colloid. It was believed that such a solution would not tend to exude so rapidly into the tissues and would therefore augment the blood volume more effectively than the fluids previously used. After many experiments it was claimed in 1916 that a blood substitute had been found in a 6 per cent. solution of gum acacia with ·9 per cent. sodium chloride. It was even stated on the evidence of laboratory experiments that the gum solution was as effective as blood in the treatment of shock and hæmorrhage. It was therefore used very extensively among the wounded, and favourable reports upon its value were made by various workers. It is difficult, however, to control the results in giving treatment of this kind. If a patient dies after being given a gum infusion, no one can state definitely that he would have lived had he been given a blood transfusion instead. If a patient lived after having a blood transfusion, it would be equally rash to state that he would have died had he been given gum. Nevertheless, after giving the gum solution a number of trials, I formed the opinion that the results were inferior to those obtained with blood. Patients did not recover whom from previous experience with blood transfusion I should have expected to do so. I accordingly continued to use blood in preference to gum whenever it was available, although justice must be done to those who so strongly advocated gum by saying that there can be no doubt that it is very much more effective than other solutions previously used. The same opinion was formed by many other surgeons, although it was natural to feel a bias in favour of gum which could be given with much greater economy of time and effort than blood. Up to the present time I have seen no reason for altering this opinion, and should always prefer to treat hæmorrhage and shock with a blood transfusion if possible.
Recently the relative values of a number of intravenous[36] infusions for shock have been put to an extensive experimental test by F. C. Mann. The shock was produced by handling the abdominal contents, and the effect on the blood pressure of the various fluids was mechanically registered. The conclusion was reached that far the best results were obtained by a transfusion of blood or blood serum, the effect of these being more permanent than that of any other substance used. The use of gum acacia was found to give results which were “variable and sometimes disastrous,” but this may have been due to some extent to errors in the technique of preparing the solution.
This draws attention to a possible objection to the use of gum, namely, that some samples of the solution have been found to be actually toxic; but it is said that this can be avoided if proper care be exercised in its preparation. Full instructions for this are given in a paper by S. V. Telfer.
Into the discussion of the relative merits of blood and gum solutions may be profitably introduced the further question as to which is the more valuable constituent of transfused blood, the corpuscles or the plasma. It has been seen that the essential factor in producing the symptoms of shock and hæmorrhage is a reduction of blood volume, and treatment is therefore directed in the first place towards the restoration of this volume, with a fluid of the same viscosity and osmotic pressure as blood. This might be done with plasma or, some may say, equally well with gum. From the point of view only of volume, the corpuscles and plasma are of equal value, since each forms approximately half the total volume of a given quantity of blood. There is, however, another aspect to be considered. One of the results of loss of blood volume is imperfect oxygenation in the tissues. When the volume is increased by the addition of plasma or gum, the corpuscles in the circulation are diluted, and this by itself would tend further to impair oxygenation. The dilution is, however, compensated for by the improvement in circulation which[37] in its turn improves the supply of oxygen to the tissues, and it is still further counteracted by the restoration to the circulation of the blood corpuscles which were stagnating in the capillary system. It seems clear that these successive processes will be accelerated by the use of a fluid which itself contains corpuscles, and this may afford a theoretical explanation of the clinical observation that blood is more effective than gum. Its use will tend to establish more quickly the “virtuous circle” following increased volume, and so undo the “vicious circle” due to insufficient volume. It has been questioned whether the corpuscles of transfused blood really do play an active part in the economy of their new host, or whether their new environment may not quickly render them effete. This has been answered by the exceedingly interesting and ingenious series of experiments carried out by Winifred Ashby. She has transfused blood of a known group (see Chapter IV) into an individual of a different, but compatible group, and then shown that it is possible by selective agglutination with a suitable serum to demonstrate the presence in the blood of the two kinds of corpuscles side by side. In this way she has shown that transfused corpuscles are still present in the circulation and of normal appearance thirty days after they were introduced.
It is therefore justifiable to make the inference that transfused corpuscles can for some little time carry out their normal function. If it be true that their presence is an advantage in the treatment of deficient blood volume, it may also be conjectured that their presence is likely to be of greater importance in treating hæmorrhage than it is in the treatment of pure shock, for in the latter condition all the original corpuscles are still present in the body, while in the former they are not.
I should sum up the discussion of the relative merits of blood and gum by saying that on the grounds of experiment and clinical experience I believe blood to be the more efficient of the two, particularly in the most serious[38] cases. Every patient who needs it should therefore have the advantages conferred by blood transfusion if it can be done. If it cannot, then gum and saline is much the most satisfactory substitute that is at present known.
Some of the concluding remarks in the foregoing pages will have suggested that the use of gum infusion may be considered of more value in treating pure shock than in treating hæmorrhage. For this reason, apart from other diagnostic considerations, it may be of importance to be able to distinguish clinically between shock and hæmorrhage. Attention has already been drawn to the fact that the symptoms and appearance seen in a patient suffering from severe shock very closely resemble those seen in hæmorrhage. It may, in fact, be impossible to say from purely clinical evidence whether a patient is suffering from shock, or hæmorrhage, or both. A case which recently came under my own observation well illustrates this point. A very stout, elderly man had fallen down a lift-shaft and was brought into St. Bartholomew’s Hospital soon after the accident. He appeared to have fallen on his feet, and the lower ends of both tibiæ had been driven through the inner sides of his soles, but there were no other signs of injury. His general condition on arrival at hospital was fairly good, but all the usual measures were taken to minimize shock. An hour or two later he had passed into a condition of extreme collapse, and exhibited all the symptoms which have already been described. Not much hæmorrhage had taken place from the wounds in his feet, and the question arose as to whether his present condition was due to internal hæmorrhage from visceral injury, or whether it was due chiefly to shock. His abdomen contained so much fat that no evidence could be obtained from an examination of it, and it was in fact impossible to arrive at any conclusion. There could, however, be no question of performing any operation, and the patient made no response to other treatment. At the autopsy it was found that there were fractures of the ribs,[39] spinal column, and symphysis pubis in addition to the injuries to the legs. There was very little hæmorrhage in connexion with any of the fractures, and it appeared that death was to be attributed almost entirely to shock. This was perhaps a somewhat unusual case, in which no help could be derived from an examination of the patient, but similar difficulties will sometimes be met.
It might be expected that a criterion would be supplied by an examination of the blood. The results from this, however, have proved to be disappointing. The facts have been investigated by Cannon and others (47) and may be summarized as follows. The number of red corpuscles in the blood from the capillaries of the ear or finger has been found to be invariably raised in patients suffering from shock. A blood count may show an increase up to seven million red cells per cmm. or even more. The blood in the venous circulation, however, of the same patient is more dilute, the count being less by one to two million red cells. When the shock is complicated by hæmorrhage, the blood count in the venous system will again be lower than that in the capillaries, but in both the counts will be less than if there were no hæmorrhage. The differences are, however, not so great or so constant that any principle can be laid down by which the two conditions may be distinguished. In patients in whom hæmorrhage is the outstanding feature the blood counts will be still lower, but the capillary and venous difference will still be present. It was found that in hæmorrhage the hæmoglobin percentage, and therefore the colour index, tended to be lower than in shock, but this was most obvious when the hæmorrhage had been very severe, and in such cases the diagnosis is usually clear from other evidences. The clinical difficulty lies in the distinction between cases of pure shock and of shock complicated by considerable hæmorrhage. It seems that little help is to be derived from an examination of the blood. This difficulty in diagnosis can only influence treatment in the direction of giving blood rather than[40] gum-saline, though the latter would probably be effective for many of the cases of shock if they could be distinguished.
The effects of transfusion for hæmorrhage and shock are to be judged best by the clinical results. The abnormal distribution of the corpuscles is altered by the treatment with a consequent redistribution in the circulation. No constant changes, therefore, in the blood count follow transfusion, and no exact mathematical effect can be demonstrated. It has been shown by Huck that sometimes the immediate rise in the blood count is greater than can be accounted for by the amount of blood given. This is often followed by a fall, which is succeeded in its turn by a second rise. These results are to be explained by alterations in the amount of destruction and formation of red cells going on in the body. That is to say, they are biological rather than mechanical, and are at present but imperfectly understood.
In the foregoing discussion hæmorrhage and shock have been considered in a general way. Something must now be said of the particular conditions for which transfusion may be given. Concerning traumatic hæmorrhage and shock there is little to be added, for these conditions present the general features of the problem in its least complicated form. No clear-cut rule can be laid down as to the point at which transfusion becomes necessary. The blood pressure is perhaps the best single indication, and if this has fallen below 80 mm. (systolic), then a transfusion is certainly indicated. Apart from this, the patient’s general condition is the safest guide. As soon as it becomes evident that his life is in danger, a transfusion should be given. Better save a few lives by many transfusions than lose them by reserving transfusion for those who are actually moribund.
Secondary hæmorrhage following an operation is fundamentally similar to primary hæmorrhage, but may present a few additional points. In recent years by far the largest[41] number of transfusions for secondary hæmorrhage have been given for bleeding from septic amputation stumps. In many cases of this sort it is no easy matter to stop the bleeding by ligaturing a bleeding vessel; sometimes it is impossible. Nevertheless, transfusion should not be withheld owing to a risk of increased hæmorrhage supposed to follow a rise in blood pressure. Usually the patient is debilitated by prolonged suppuration, and often his blood is deficient in its power of coagulation. It has been found that a transfusion, in addition to replacing some of the blood that has been lost, tends to improve the patient’s resistance to micro-organisms, and to shorten the coagulation time of the blood. Recurrence of the hæmorrhage is therefore discouraged on the whole, and in many cases a series of transfusions for recurrent hæmorrhages has saved a patient’s life when the prognosis had seemed to be almost hopeless.
Post-operative hæmorrhage associated with chronic jaundice is another condition which demands special consideration; this will be dealt with later under the heading of hæmorrhagic diseases.
The proper treatment of severe hæmorrhage from a gastric or duodenal ulcer has always puzzled physicians and surgeons alike. It is probably true that patients very seldom die as the result of a single rapid hæmorrhage, even if severe. There can, however, be no doubt that death due actually to acute anæmia may follow repeated or prolonged hæmorrhage. Hitherto treatment has been conducted mainly on medical lines. Opinion is now, however, tending to favour earlier and more frequent surgical interference, and this can be made a less dangerous procedure by giving a preliminary blood transfusion to improve the patient’s general condition. When the patient’s life is threatened by hæmorrhage repeated or prolonged, transfusion is undoubtedly the best means of saving him. Here again the fear of restarting the hæmorrhage by raising the blood pressure has acted as a deterrent, so that transfusion[42] is apt to be withheld until too late. Nevertheless, it is clear from the numerous cases recorded in the literature that this fear is groundless (130, 215, etc.). The effect of a transfusion on the coagulating power of the patient’s blood more than compensates for the risk attending a rise in blood pressure. Now only is lost blood replaced, but also the clot plugging the damaged vessel is made more secure. The patient is tided over the immediate danger to his life, and surgical treatment is made possible. This view will doubtless meet with much adverse criticism, but its justice will eventually be recognized.
As in the early days of transfusion, so at the present time, a considerable proportion of the patients that need transfusion will be met with in the course of obstetrical practice. It has often been remarked how much blood can be lost by a woman following the delivery of her child without any serious result; nevertheless, many deaths are occasioned every year by post-partum hæmorrhage, placenta prævia, and rupture of an ectopic gestation. Sometimes the bleeding is so rapid that there is no margin of time available for a transfusion unless all the facilities be immediately at hand. Short of this, transfusion is the ideal treatment, and the problem is a simple one, the relief of acute anæmia being the only object in view. One interesting modification of the procedure has been recently recommended by German writers, namely, the reinfusion of the patient’s own blood. This is applicable only when the hæmorrhage has taken place into the peritoneal cavity, and is therefore limited to the treatment of a ruptured liver or spleen, a ruptured uterus, or a tubal abortion. With a ruptured uterus the sterility of the blood is not assured, and this condition were better not included. For the other conditions Lichtenstein recommends that the blood should be ladled out of the peritoneal cavity into Ringer’s solution and then strained to remove clots. The resulting fluid is infused into a vein. Judging from my own experience of intraperitoneal hæmorrhage, not much[43] blood would actually be recovered in this way, since usually so much of it has clotted. In any case, the whole procedure is to be looked upon with suspicion owing to the unknown and probably profound changes that have taken place in partially clotted blood. Eberle records that in one case reinfusion was followed by hæmolysis, and among twenty-one cases reported by Schweitzer in 1921, one death was attributed to the reinfusion, which, as in Eberle’s case, was followed by hæmoglobinuria. Transfusion has also been used for the toxæmias of pregnancy, but this will be dealt with under another heading.
[44]
It is claimed that blood transfusion provides an efficient means of treatment in most conditions distinguished by symptoms of spontaneous hæmorrhage or by traumatic hæmorrhage which cannot be controlled. All such diseases have the common features that the coagulation time of the blood is abnormally prolonged, and it may be supposed that the transfused blood supplies some missing constituent, so that for the time the blood is enabled to coagulate more normally. Most of the evidence available shows that the claims made for transfusion are not exaggerated.
Jaundice.—It is well known how exceedingly dangerous an operation upon a jaundiced patient may be owing to the difficulty of obtaining hæmostasis. The coagulation time of the patient’s blood is not affected in a transient catarrhal jaundice, but in the chronic condition it has been shown to be three or four times the normal (223). In these circumstances it is found that a transfusion is of some use in shortening the coagulation time of the patient’s blood so that bleeding ceases, although sometimes, especially in cases of jaundice due to malignant disease in which the biliary obstruction has not been relieved by the operation, the effect is very transitory, and after two or three days the patient may again begin to bleed (215). No other method of overcoming this has yet been found to be more effective than transfusion, though the intravenous administration of calcium compounds is sometimes of value.
[45]
Hæmophilia.—Blood transfusion is of still greater value when the coagulation time of the blood is prolonged owing to a congenital deficiency, as in hæmophilia. It is unnecessary to discuss here in detail the precise nature of the deficiency. No definite conclusion has yet been reached, though it seems to be clear that the abnormality resides in the organic clotting complex, and not in the calcium content of the blood. Treatment, therefore, will aim at supplying the deficient substance, so that the coagulation time may be reduced to normal, whereupon the bleeding will cease. Various methods of bringing this about have been used. Horse serum or whole blood injected subcutaneously has often been found effective and sometimes even when used merely as a local application. Not infrequently, however, horse serum fails of its effect, so that no reliance can be placed upon it. Even when effective, the alteration in coagulation time is transitory, a fact which introduces an obvious objection to its use, for if the occasion should arise, as it easily may, for a repetition of the treatment, the patient may be exposed to the risk of severe anaphylactic shock.
Another form of treatment has been introduced by H. W. C. Vines, in which a slight anaphylactic shock is deliberately induced, the result of this being a fall in the coagulation time of the blood to normal. The mechanism of this change is at present unexplained. Again, the effect is transitory, but for a certain period afterwards a surgical operation may be safely performed upon a hæmophilic patient treated in this way. This method has not yet been extensively tested, and in any case it cannot be used in an emergency, for the patient must be sensitized by a preliminary injection and an interval of several days allowed to elapse before the anaphylaxis can be produced.
The efficiency of blood transfusion in the treatment of hæmophilia has been very often demonstrated, and seems at present to afford the most certain means that we possess of arresting the symptoms. Presumably the transfused[46] blood supplies directly the deficient factor in the coagulation complex, and it has been shown by Bernheim (1917) that the transfusion even of quite a small amount of blood will almost immediately stop the bleeding. In addition to comparative certainty and rapidity in action, transfusion has the advantage that it will replace the blood which has been lost, for often the patient has reached a stage at which he is in danger of his life from actual anæmia. This treatment, therefore, will always be useful in an emergency, whether the patient be bleeding to death from a slight wound, or whether he be suffering from acute appendicitis and so is in need of an immediate operation. If transfusion does not at once stop the bleeding, the treatment can be repeated, so that the patient should not be allowed to die from loss of blood. In most cases the bleeding will eventually stop if the patient’s life can be prolonged. Even if the treatment be immediately successful, the transfused blood necessarily contains only a limited quantity of the substance necessary for the coagulation complex, and this gradually disappears. Again, therefore, the effect is transitory, so that transfusion is in no sense curative. It has been noticed that the tendency of a hæmophilic to bleed decreases as age advances, and it has been suggested by Ottenberg and Libmann that small quantities of blood should be injected into his veins at regular intervals of one to three months. It is possible that in this way he might be brought safely through the more perilous years of his life.
The proof of the effect of transfusion upon the coagulation time of the blood rests upon the evidence of a number of independent observers. Pemberton has recorded a case of a hæmophilic whose coagulation time before transfusion was estimated to be 23 minutes. Blood was given to the amount of 500 cc., and 5 minutes later the coagulation time was 3 minutes. Twelve hours later it was 8 minutes, and on the fourth day after transfusion it had risen again to 20 minutes.
[47]
Other observations have been made as follows:
| Coagulation time. | Minutes. | |
| Bulger | Before transfusion | 82 |
| 1 day after transfusion | 10 | |
| 8 days ” ” | 8 | |
| 25 ” ” ” | 40 | |
| Minot & Lee | Before transfusion | 150 |
| After ” | normal | |
| 3 days after transfusion | 60 | |
| 5 ” ” ” | 100 | |
| Addis | Before transfusion | 245 |
| After ” | 24 | |
| 25 days after transfusion | 200 | |
| After 8 cc. serum injected | 38 | |
In treating jaundice or hæmophilia the transfusion may be performed by the method of choice described in Chapter VII of the present work. The addition of an anticoagulant to the blood does not render it any less efficient as a hæmostatic agent. In all cases the coagulation time of the patient’s blood is found to be reduced after transfusion, whether sodium citrate be used as an anticoagulant or not. The explanation of this may be found in the fact referred to on p. 120, that the citrate is very rapidly destroyed in the circulation, and so cannot for long influence adversely the hæmostatic properties of normal blood.
The seeming paradox of using an anticoagulant in an endeavour to promote the coagulation of the blood is heightened by the work of Ottenberg, who has shown that the coagulation time may be reduced by the intravenous injection of sodium citrate alone. In this experiment 20 cc. of a 3 per cent. solution of sodium citrate were injected into a hæmophilic, whose coagulation time had been found to be 85 minutes. Ten minutes after the injection it was found to be 25 minutes. Two days later it had risen again[48] to 85 minutes. This observation has not been confirmed but, if it be true, citrated blood is likely to be actually more efficient in the treatment of hæmophilia than untreated blood.
The amount of blood to be transfused in hæmophilia will vary with the age of the patient and according to whether he is suffering from acute anæmia or not. If hæmostatic effects only are wanted, 100 cc. of blood will be enough. If anæmia is also present, the dosage will be governed by the same considerations as have already been discussed in the section on the treatment of hæmorrhage.
Melæna Neonatorum.—Another hæmorrhagic condition in which blood transfusion is of the very greatest value is that known as melæna neonatorum. Severe hæmorrhage takes place from the bowel of an infant, sometimes only a few hours after birth. The cause is quite unknown, but it is found that absolute hæmostasis is usually brought about by blood transfusion. Horse serum has often been successfully used as in treating hæmophilia, but blood transfusion again has the additional merit that the blood which has been lost is thereby replaced. A single transfusion is usually enough, as the hæmorrhage does not tend to recur when once it has been stopped. For a newly born infant, even if in extremis, only a small quantity of blood is needed, so that a transfusion of 50 to 100 cc. is usually found to be enough. Bruce Robertson suggests that, as a good working rule, the amount should not exceed 15 ccm. per pound of body weight. The superficial veins of an infant are exceedingly small, so that the introduction even of a fine needle into the median basilic may be matter of the greatest difficulty. The best method of transfusing an infant, therefore, demands special consideration. A description of this will be found on p. 134 of the present work.
The value of transfusion for melæna neonatorum has not been very generally recognized, but a number of striking[49] cases have been reported. Defibrinated blood had been used in 1873 by Sir Thomas Smith as described in Chapter I, but the first case in which whole blood was used was published by Lambert in 1908. Later, in 1910, Welch, and then Schloss, recommended the subcutaneous injection of serum or of blood, but these measures were clearly not so effective as the intravenous transfusion of blood, as has been testified by numerous observers (Lespinasse, Unger, Vincent, Graham, Bruce Robertson, Lapage, Hutchinson, etc.). The patients may be actually moribund, for a new-born infant can only afford to lose a relatively small amount of blood, but even then transfusion is often successful. Bruce Robertson reports that of a series of forty cases of hæmorrhagic disease of the new-born which were treated by transfusion, all recovered except four; of these two died from associated umbilical sepsis, one from intracranial hæmorrhage, and the fourth had already ceased breathing when the treatment was begun.
It has sometimes been stated that for transfusing an infant either parent can be safely used as blood donor, on the assumption that the serum reactions are not yet developed. This may sometimes be true, but the fallacies and possible dangers of this are explained in a later chapter.
A case was recently reported by R. D. Laurie, who, knowing that he himself belonged to Group IV, drew 20 ccm. of his own blood into a syringe containing five grains of sodium citrate in solution. This he injected into a vein in the infant’s arm; the small size of the vein he had chosen made this difficult, but the treatment resulted in the rapid recovery of the patient.
Purpura.—Of all the forms of hæmorrhagic diseases, the two already described, hæmophilia and melæna neonatorum, are the only ones for which blood transfusion is a really effective remedy. It is probable that under the somewhat general term “purpura hæmorrhagica” are grouped several conditions, all of very obscure origin, none of[50] which are conspicuously benefited by transfusion. Many transfusions have been given for purpuric symptoms, chiefly in America. Several cases are reported by Bernheim, and twelve transfusions were given to seven patients by Peterson. In some of these the treatment produced a temporary improvement, but usually they relapsed after an interval of a few months. One of Bernheim’s patients appears to have owed his life for the time being to a transfusion, but he died subsequently during a recurrence. Two cases are reported by Graham. One was not benefited at all; the other improved for a time, but afterwards relapsed. In a serious case, therefore, transfusion may be worth trying; it has indeed been stated by Ottenberg and Libmann, observers with a wide experience of transfusion, that this treatment is “definitely curative” in severe cases of purpura. At the present time there is little to add on the subject, but it is possible that further advances will be made by proceeding on these lines.
Pernicious Anæmia.—Blood transfusion has been advocated for several conditions characterized by alterations in the cells of the patient’s blood. It has been used in the treatment of aplastic anæmia, splenic anæmia, chlorosis, and leukæmia, but in none of these diseases has it been of much avail. In pernicious anæmia, however, transfusion has proved to be of very great service.
It is, indeed, now a recognized form of treatment for this disease, though the numerous reports upon results that have been published have not pronounced unanimously in its favour. Variability in results probably depends to some extent upon the difficulty of distinguishing true pernicious anæmia from some forms of secondary anæmia. It is hardly to be expected that much benefit would follow blood transfusion in the undiagnosed secondary type, since the destruction or loss of corpuscles is continuous[51] until the cause has been removed. In true pernicious anæmia, on the other hand, there may be remissions in the disease, and it is quite clear that these may be initiated or prolonged by blood transfusion. The largest number of consecutive cases that has been recorded was treated in the Mayo Clinic in the years 1915 to 1918 (Archibald, Pemberton, Hunt). It was estimated that in about 60 per cent. of the patients with pernicious anæmia a definite improvement followed transfusion. It is generally agreed that the best results are seen in those who have not yet reached the last stages of the disease, though sometimes patients who are actually in extremis will also show great improvement. A remarkable instance of this has been reported in Norway (261). A man, aged thirty-three, was dyspnœic, semi-conscious, and moribund when admitted to hospital. His red cells numbered 850,000 per cmm., and his hæmoglobin percentage was 19. Immediate improvement followed the transfusion of 900 cc. of citrated blood, the red cells rising quickly to 2,000,000 and later to 3,000,000. Twelve days after admission he was walking about. No case must therefore be regarded as hopeless, though disappointments must be expected.
As a general rule blood transfusion should be given before the more serious secondary manifestations of the disease have shown themselves, that is to say, some time before the condition has become dangerous to life. Probably the disappointing results of this treatment have partly been due to the fact that it has been regarded as a last resort and has often been given at too late a stage. No rule can be laid down as to when transfusion should be given, but common sense suggests that it should be tried as soon as it is evident that the disease is progressing in spite of other methods of treatment. One authority (Anders) even advises that transfusions should be given as soon as an assured diagnosis has been made, but he weakens his case by adding that other methods of treatment should be used at the same time. If the patient is already seriously[52] ill when first seen, the blood transfusion should be tried at once, as its effect, if beneficial, is likely to be more rapid than that of any other form of treatment.
The amounts of blood given in pernicious anæmia have varied. Massive doses have occasionally been given (179), but the general opinion seems to favour smaller amounts, 300-500 cc., the dose being repeated at intervals of two or three weeks. Repeated transfusions have been an outstanding feature of the treatment, and as many as thirty-five transfusions of 500 cc. or more have been given to one patient, extending over a period of thirty months. This is in itself a demonstration of the fact that blood transfusion does not cure the disease; the beneficial effect of each transfusion may wear off in a short time, but by repeating the treatment the patient’s life can be prolonged for months or even years beyond the time when it would otherwise have ended.
Although the effect of transfusion is apt to be transient yet it is certain that its good effects are due not merely to the addition of a certain number of healthy corpuscles to the circulation, but, in addition, to an obscurer factor. This can best be expressed by saying that the transfused blood appears to have a stimulating effect upon the blood-forming tissues of the patient, so that more red corpuscles are discharged into the circulation. One observer believes that enumeration of the reticulated red cells may be used as an indication of the hæmopoietic powers of the bone marrow (289). The reticulated appearance is assumed to be characteristic of cells which have recently entered the circulation. The mode in which this stimulus acts is unknown, and the whole subject calls for further investigation. That this does take place is well illustrated by the following details of three cases from Dr. Drysdale’s wards at St. Bartholomew’s Hospital. The transfusions were given by Dr. Joekes, who was also responsible for the estimations of the corpuscles.
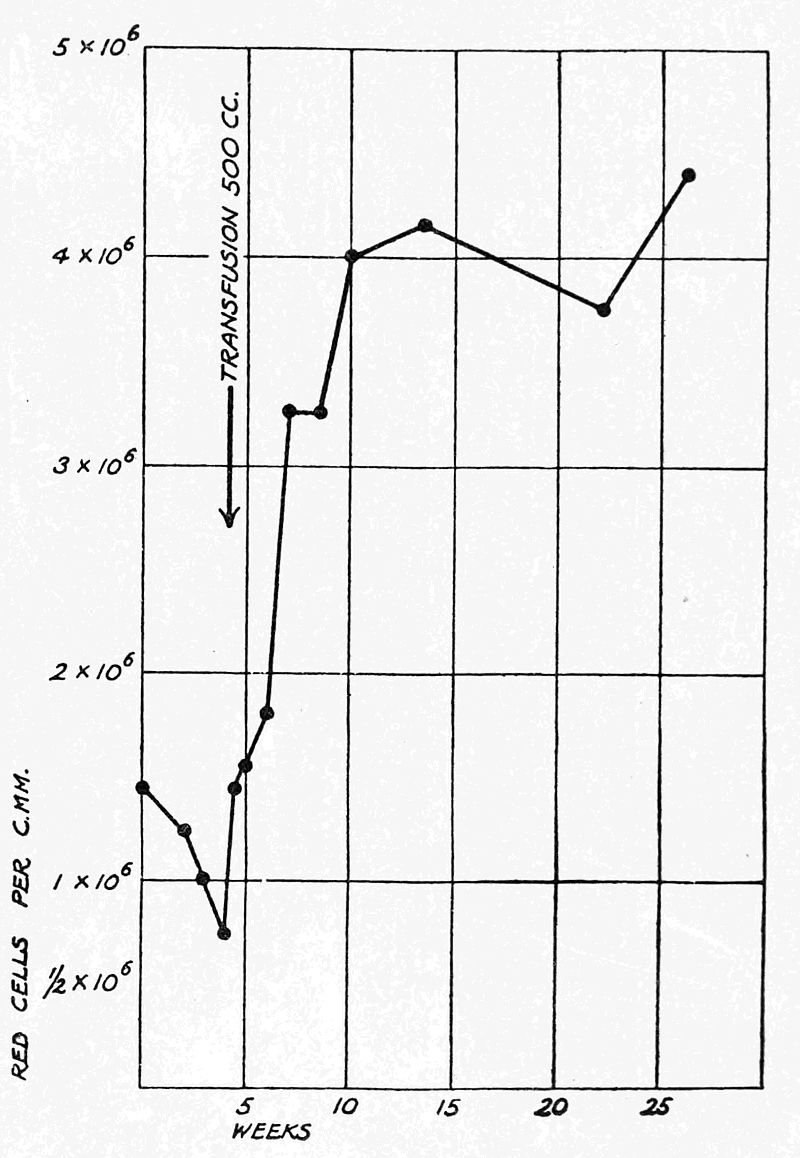
I. A woman, aged 51, had been treated for four years for[53] pernicious anæmia, and when admitted to hospital was becoming steadily worse. The red corpuscles numbered 1,470,000 per cmm., and her hæmoglobin percentage was 32 on October 21, 1918, and by November 19 they had fallen to 750,000 and 25. On November 22 she was transfused with 500 cc. of citrated blood, and a blood count made immediately afterwards showed that she then had 1,410,000 red cells per cmm. On December 12 the number had risen to over 3,000,000, and on January 28 of the following year it was over 4,000,000. This was still maintained in May, 1919, and on the last occasion on which a blood count was made she was found to have 4,400,000, with a hæmoglobin percentage of 90. Since then she has been lost sight of, but would certainly have returned had she relapsed. This case shows what remarkable results sometimes follow a single transfusion and the progressive improvement[54] which follows the initial rise. The diagram shows the results more graphically.
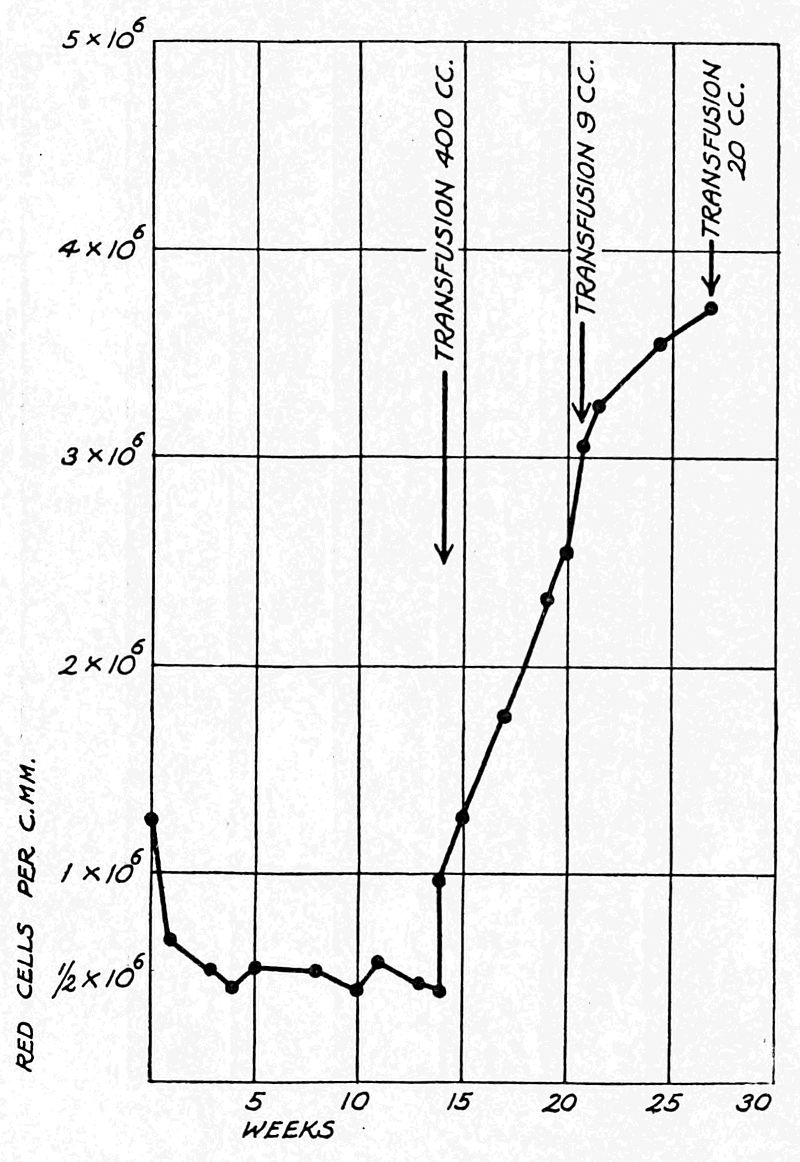
II. A similar result, even more striking, was obtained in a woman aged 42. She was treated medicinally for four months, during which time her red cells steadily decreased from 1,250,000 to 429,000 per cmm. She was then transfused with 400 cc. of blood, and her blood count rose immediately to 967,000. The rise continued steadily, and three months later her blood count was 3,690,000 per cmm. Two very small additional transfusions were given during this period, but to what extent these helped in the treatment cannot be estimated. The results in this case also are represented graphically by the diagram above.
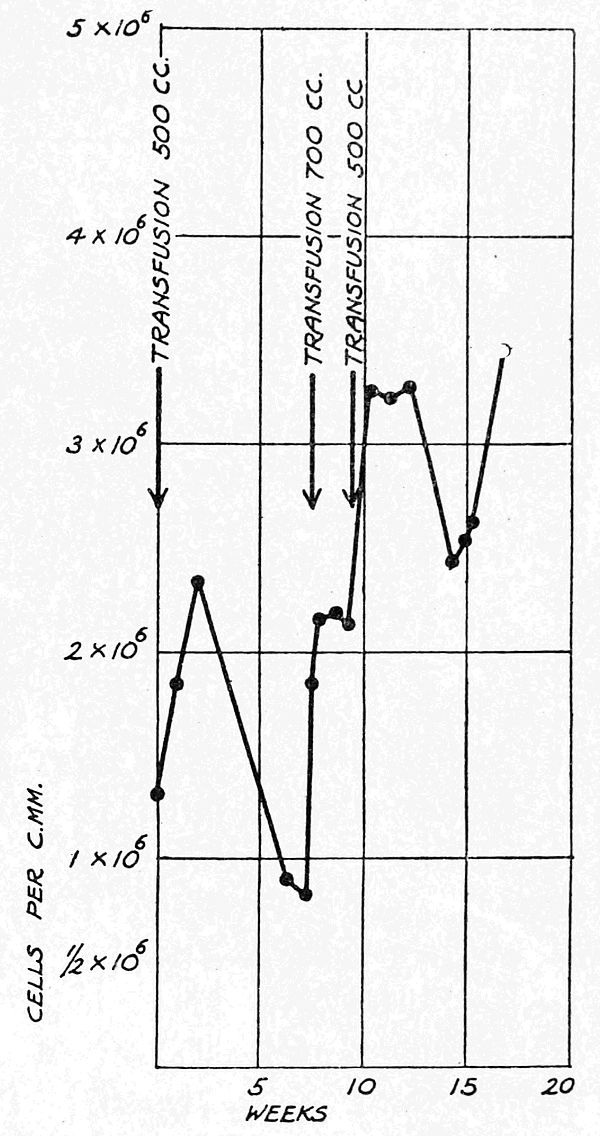
III. A less favourable result is illustrated by the following history: A stores assistant, aged 47, had been ill for two years, and was first treated for pernicious anæmia in[55] April, 1920. He was medicinally treated with arsenic, but no improvement followed. On June 18, 1920, his corpuscles numbered 1,060,000 per cmm. He was transfused with 600 cc. of blood, and his corpuscles increased at once to 1,840,000 per cmm. A month later there had been a further increase to 2,520,000, but this was not maintained, and nine months afterwards he was given a second transfusion of 500 cc. of blood. Immediately after this his red cells numbered 1,800,000 per cmm. (April 14, 1921). There was a further slight rise and then another rapid fall, so that on June 4, 1921, he had only 830,000 red cells per cmm. He was then given a third transfusion of 700 cc. The effect of this was a steady rise, and on June 17 he had 2,112,000 red cells per cmm. A fourth transfusion of 500 cc. was given at this point, and thereafter the improvement was maintained, with slight variations, until, on August 4, 1921, his corpuscles numbered 3,450,000 per cmm.
In this case the effect of the two first transfusions was short-lived, but perseverance with the treatment brought him in the course of two months from an extremely serious condition to a state of comparatively good health, in which[56] he could again for a time go about his business. The diagram illustrates well the rise which followed each of the later transfusions. He had again relapsed four months later, but, unless each transfusion had chanced to coincide with the remissions which may occur spontaneously in this disease, it seems clear that the treatment greatly relieved him for a time.
There is no objection to the use of citrated blood for pernicious anæmia, so that the transfusion can be carried out in the ordinary way described in Chapter VII. It is necessary, however, to utter a warning as to the choice of a blood donor. It is quite clear that in some patients, whose disease has been diagnosed as pernicious anæmia, there is an alteration in the reactions of the serum. The corpuscles may show an agglutination which conforms to one of the group tests described in Chapter VI; nevertheless, it is essential in addition that the patient’s serum should be tested directly against the corpuscles of the proposed donor, even if he belongs to Group IV, whose corpuscles are not agglutinated by the serum of any normal person. I was recently asked to transfuse a patient whose disease had been diagnosed as pernicious anæmia. Her red blood cells had fallen to 600,000 per cmm., so that she was probably in the last stages. Her corpuscles were agglutinated only by serum of Group III, so that she apparently belonged to Group II. Only two donors were available, both of whom belonged to Group IV. Nevertheless, the patient’s serum strongly agglutinated the corpuscles of both of them, so that I considered it inadvisable to carry out the treatment. Similar abnormalities have been noticed by others. It seems to be a universal experience that slight reactions are more commonly met with after transfusion for pernicious anæmia than when it is done for other conditions, although these do not in any way prejudice the results that are obtained. These reactions are possibly to be explained by abnormalities, though of slight degree, in the patient’s serum. In a case[57] such as I have described the reaction would probably be very severe, if not fatal. It is possible also that a well-marked alteration in the serum reaction is not characteristic of the clinical entity constituting true pernicious anæmia, but in reality indicates that there is another underlying cause for the anæmia, such as an undiagnosed carcinoma. Dr. Joekes has recently (August 1921) told me that he believes from his own observations that this is actually the case, but it needs to be established by further investigation. The connexion between malignant disease and abnormal serum reactions is referred to elsewhere (p. 93).
Another possible complication is introduced into the treatment by the necessity for giving repeated transfusions. It has been noticed that sometimes a serious reaction follows one or more of the later transfusions of a series, even when the blood is taken from the same donor who had been used before without ill effects. A report on several such cases shows that this form of reaction cannot be predicted or eliminated by the most careful testing beforehand for reactions between the patient’s serum and the donor’s corpuscles, though it has occasionally been so severe as actually to hasten the patient’s death (34). This fact suggests that the reaction is not due to the presence of agglutinins, but is rather of the nature of an anaphylactic shock, the patient having been sensitized by a trace of foreign protein introduced in the blood on the earlier occasions. Possibly it may be to some extent avoided by not using the same donor if another is available. It also emphasizes the necessity for giving the blood slowly and cautiously, so that the transfusion may be stopped at the first sign of a reaction in the patient.
Very large numbers of transfusions for pernicious anæmia have been given in the past, yet a reaction of a dangerous severity has occurred in but few of them. This need not, therefore, be regarded as a contra-indication for transfusion, but rather as an indication for circumspection[58] in giving it. Transfusion is clearly a therapeutic measure of great value.
Very recently it has been claimed by Waag that excellent results have been obtained by the repeated subcutaneous injection of small doses (5 cc.) of whole blood. In an actual case which he reports, nine injections were given twice weekly. If the claim be substantiated by further successes, this method of treatment may eventually supplant the more elaborate process of actual transfusion.
Pyogenic.—The value of vaccines and bactericidal sera in pyogenic infections, though not in universal favour, is strongly advocated by many competent authorities, and the transfusion of blood from an immunized donor suggests itself as a natural corollary. A quantity of blood taken from a vigorously reacting man and given to a debilitated patient should theoretically supply him with a large amount of the antibodies of which he stands in need. During the war it was found that transfusion enabled an exsanguinated patient better to withstand the attacks of pyogenic and putrefactive organisms in his wounds, but this was probably due to the improvement in the general circulation which resulted rather than to any bactericidal properties in the transfused blood. It is known that outside the body blood has considerable powers of inhibiting the growth of bacteria, but ordinarily it does not possess bactericidal properties. It has been claimed, on the other hand, that the best criterion of the degree of immunity in an immunized animal is the measurement of the bactericidal power of its blood. There is justification therefore for attempting to combat a pyogenic infection by the transfusion of immunized blood.
This method has at present not progressed beyond the stage of preliminary trials. I have attempted it in one[59] case, but without any obvious benefit. The patient was a middle-aged man suffering from a chronic staphylococcal septicæmia and a secondary anæmia. He received a transfusion of 650 cc. of blood from a donor who had himself just recovered from a severe infection with staphylococcus aureus. The patient’s red blood cells underwent a temporary increase in number, but no other result was observed. One series of nine cases has been recorded by Fry, and in these the results leave some doubt as to the efficacy of the treatment. Six of these patients were almost hopelessly ill with streptococcal (five) or staphylococcal (one) septicæmia, and only one of these responded to treatment. He received transfusion from an ordinary donor and two from immunized donors, who had been given five or six injections of a mixed vaccine, the maximum dose of which contained 120,000,000 streptococci. Improvement definitely followed the transfusions, and his recovery was afterwards encouraged by injections of an autogenous vaccine. The other five patients received similar treatment, but all died. The remaining three patients had chronic suppuration, one following a streptococcal arthritis of the knee, but no septicæmia, and all recovered. It cannot be assumed that these recoveries were due to the transfusions.
It is stated by Waugh that he transfused nineteen cases of pyæmia of whom twelve recovered, and in these cases an ordinary donor was used. No details, however, are given, so that it is not possible to make any inferences from this.
Greater success is claimed by Hooker, who reported that in five cases of pyogenic infection the results were distinctly favourable. He used immunized blood, but has formed the impression that the transfusion even of normal blood is of value in septicæmia by correcting the anæmia and helping to restore the normal resistance. He recommends that if the patient has a good blood volume and a high bacterial content in the blood, he should be bled by[60] venesection before transfusion. A striking case of staphylococcal septicæmia has been recorded by Little, who believed that the patient’s recovery was directly due to the treatment. Four transfusions were given, the blood for three of these being taken from donors who had each received, four days previously, an injection of vaccine made from the patient’s own infection. Ottenberg and Libmann have treated ten cases of pyogenic infections with transfusions. All the patients were extremely ill and six died. It is stated that the four who recovered “probably owe their lives to the transfusion,” but obviously it is difficult to control the results. The same observers have used transfusion in the treatment of infective endocarditis, but unsuccessfully.
Some experimental work on this subject has been carried out by Kahn. A bacterial infection was introduced into the peritoneal cavities of several dogs. Continuous transfusion between an infected dog and a healthy dog was then performed, the blood passing to and fro between the animals, sometimes for over an hour. It was found that all the transfused animals fared better than those that were not. The experiment suggests that resistance to infection is heightened if two bodies can combat the infection present in one; but continuous transfusion is scarcely practicable in man.
Diphtheria.—In the later stages of some acute diseases due to a bacterial infection, the patient falls into a condition of acute toxæmia, the symptoms of which resemble in some ways those of shock. Harding has drawn attention to this condition in diphtheria; he has produced it experimentally in animals and has treated it by blood transfusion. The toxæmic stage was found to occur on the fourth to the eleventh day. It was characterized by a reduction of the output of the heart with a corresponding fall in blood pressure, an exudation of lymph into the tissues, and an increased specific gravity of the blood. In all these respects it resembled the collapse due[61] to trauma or to hæmorrhage, and it was shown by experiment that the treatment must be directed towards increasing the amount of effective fluid in the circulation and to decreasing its viscosity. It was found that normal saline solution failed to do this; gum-saline solution also failed, and tended to produce a pronounced agglutination of the red blood cells. Blood transfusion, on the other hand, resulted in a considerable number of recoveries. In the aggregate more than twice as many animals survived after transfusion as survived without it, the same amount of toxin being given in each case.
These experimental findings are exceedingly suggestive, but the clinical efficacy of the treatment still remains to be proved. Harding found that the amount of blood that should be transfused was one-fifth of the total blood volume; the following amounts are, therefore, recommended for the treatment of children in the toxæmia stage of diphtheria:
| Age. | Weight. | Amount. |
| 1½ years. | 21 lbs. | 160 ccm. |
| 2 ” | 28 ” | 200 ” |
| 4 ” | 35 ” | 300 ” |
| 6 ” | 42 ” | 400 ” |
Pneumonia.—A condition of toxæmia similar to that seen in diphtheria was also observed in some of the cases of pneumonia which complicated the influenza epidemic of 1918-19. In the United States, among a large number of cases admitted to an emergency hospital, a series of 28 patients, some of whom were moribund, was treated by blood transfusion by Rose and Hund. The results were compared with those in 21 similar cases which were not transfused. The figures seemed to show that transfusion was of some value. Of the 28 who were transfused, 6, or 22·4 per cent., died, and the rest recovered; of the 21 who[62] were not transfused, 9, or 47·7 per cent., died, and 12 recovered. The numbers treated are not large enough to afford statistical evidence that can be relied upon, but the results were at least encouraging.
Typhoid, Measles, Tuberculosis.—Transfusion has been tried for several other bacterial infections with varying results. McClure has administered immunized blood to a typhoid patient with a remarkably good result. Ottenberg and Libmann have transfused five typhoid patients, all of whom were desperately ill; two of them recovered. Transfusion has also been used for intestinal hæmorrhage in typhoid, but this is chiefly with the object of combating anæmia. Subcutaneous injection of blood has been successfully used by Terrien in a case of malignant measles; the donor had had measles six months previously. Freilich has recently transfused six patients suffering from tuberculosis, but without benefit. He is at present testing the use of blood from donors who show a positive complement fixation test for the tubercle bacillus.
It is evident that treatment with immunized blood is still in an experimental stage, but it merits further trials, all the circumstances of which should be carefully recorded.
Toxæmias of Pregnancy.—The treatment of eclampsia by blood transfusion was first employed by Kimpton, who speaks favourably of the results obtained. Later it was independently suggested to Blair Bell, who was the first to employ it in this country, by certain investigations into the facts of immunology. It had been found that symptoms resembling those of eclampsia could be produced in mice by injecting into them an extract of placenta, whether from a healthy or an eclamptic woman; the same results were obtained by injecting fresh serum from similar individuals. Further, if the placental extract was mixed with serum from a normal person of either sex, the effects were not obtained, and it was inferred that the placental toxin had been neutralized by antibodies in the serum. If, however, the placental extract was mixed with serum[63] obtained from the blood of an eclamptic patient, then the toxic symptoms were obtained as before. Apparently, therefore, the serum in eclampsia lacks certain antibodies which are present in the serum of normal individuals. If these observations had been correctly interpreted, it seemed reasonable to suppose that blood from a normal person would supply an eclamptic patient with the antibodies which she lacks. The patient treated by Blair Bell was already comatose and apparently dying. She was given 500 cc. of citrated blood and rapidly recovered; her convalescence was uninterrupted. It would be unwise to found great hopes on a single case, but the treatment undoubtedly merits further trial.
Transfusion has also been used by Keator in treating the toxæmia of early pregnancy, and Morel has successfully used the blood of a healthy pregnant woman for the same purpose. Gettler recommends the use of alkalinized blood for “acidosis” in pregnancy. At present, however, little evidence can be adduced in favour of this form of treatment.
Nephritis.—A single case of nephritis successfully treated by blood transfusion has been recorded by Ramsay. The patient, a man aged 22, had been ill for ten days. He was slightly drowsy and had a furred tongue. His systolic blood pressure was 100 mm. and diastolic 60. His urine had a specific gravity of 1010, and contained much albumin and many granular casts, but no blood cells. Vomiting was incessant. On the second day after admission he passed 2 ozs. of urine and his systolic blood pressure fell to 90 mm., his diastolic to 40 mm. His low blood pressure and the evident imminence of suppression of urine suggested the administration of blood; he was accordingly given 1,140 cc. of fresh blood. His blood pressure immediately rose to 100 mm. systolic, and 50 mm. diastolic, and the other symptoms abated. He passed 24 ozs. of urine during the ensuing twenty-four hours. He was afterwards treated with alkalies, intravenously and[64] by the mouth, and his condition steadily improved. It cannot be inferred from the evidence that his recovery is to be attributed entirely to the transfusion, but it appears to have been initiated by this treatment, which was a reasonable one in view of the symptoms. No other similar cases have as yet been recorded.
Carbon Monoxide Poisoning.—In any condition in which the function of a large proportion of the red blood cells as oxygen carriers has been temporarily destroyed or impaired, it is a rational procedure to replace as many of them as possible with normal red cells. The evidence that transfused blood cells can carry out their functions in their new host has been given on another page. In carbon monoxide poisoning the oxyhæmoglobin has been converted into carboxyhæmoglobin, which is more stable than the oxygen compound, and therefore useless for purposes of respiratory exchange. Undoubtedly the ideal treatment for carbon monoxide poisoning is by putting the patient in a specially constructed chamber in which he can breathe oxygen under a pressure of about three atmospheres. By this means the carboxyhæmoglobin is dissociated and replaced by oxyhæmoglobin. An oxygen chamber is usually not available, though a very useful substitute may be tried in the shape of a Haldane’s oxygen mask. Failing this, there is evidence to show that a blood transfusion is an effective form of treatment. Nevertheless, although poisoning with coal gas is by no means a rare event, this treatment does not seem to have had the attention it undoubtedly deserves. Transfusion was first used for carbon monoxide poisoning by Hüter in 1870, who was able to record a case in which recovery appeared to have been due to the treatment. It was also advocated by Lauder Brunton in 1873. After this date recorded cases are few, but in 1916 Burmeister put this form of treatment on a more scientific basis by direct experiment. Using rabbits and dogs he showed that if the animals treated with coal gas were transfused without a venesection, 75 per cent.[65] of them recovered. Of a series of control animals, which were not transfused, nearly all died.
Most writers on the subject have recommended that as much blood be taken from the patient by venesection as is to be replaced by transfusion. On theoretical grounds this seems to be sound, though it is not supported by the results of Burmeister’s experiments. Nevertheless, in a recent series of seven cases reported by Bruce Robertson, in which 1,000 cc. of blood were removed and the same amount given by transfusion, satisfactory results were obtained. If no venesection is done, there is some risk that the transfusion may put an additional load upon an already over-strained right heart, so that a preliminary venesection is certainly a wise precaution. Transfusion should not be withheld until the patient is in extremis; if no oxygen chamber is available, it should be given at once. A minimum amount of 750 cc. of blood should be taken by venesection, and 1,000 cc. of blood should be given. If the patient’s condition does not then show enough improvement, this should be repeated.
Nitrobenzol and Benzol Poisoning.—Blood transfusion for poisoning with nitro-benzol (C6H5NO2) has been recommended by Hindse-Nielsen, who records a case in which it was successfully employed. The patient, a girl of 19, had taken a tablespoonful of the poison several hours before, and her condition appeared to be hopeless. She was deeply cyanosed, the mucous membranes being of a dark blue colour. Washing out the stomach and inhalation of oxygen were tried without effect. Finally she was bled to the extent of 600 cc., and 1,000 cc. of citrated blood were injected. Her colour at once became more normal and recovery followed. The literature does not contain records of any other cases treated in this way, but the condition is analogous to coal-gas poisoning referred to in the last paragraph, oxyhæmoglobin being in this case replaced by methhæmoglobin, and its treatment by transfusion has, therefore, a rational basis.
[66]
A somewhat similar condition is seen in benzol poisoning, though there is an additional destruction of red blood cells. Three cases treated by transfusion have been reported by McClure. One patient, whose red blood cells had been reduced to 1,460,000 per cmm., was extremely ill, but recovered after five transfusions up to a total amount of 1,500 cc.
Diabetes.—Blood transfusion has been used in treating diabetes mellitus, but there is no evidence to show that it is of any service. Ottenberg and Libmann transfused four patients who were already in diabetic coma, but no improvement resulted. Another patient who was transfused by Raulston was actually made worse, as was indicated by an increased output of sugar, acetone, and ammonia compounds.
Pellagra.—The precise ætiology of pellagra being still unknown, treatment of the disease can only be empirical. From this point of view blood transfusion has been tried by Cole, who began using it in 1908. The results in twenty cases have been reported, and are distinctly encouraging. All the transfused patients were in the last stages of the disease, but nevertheless a recovery rate of 60 per cent. was obtained, the usual rate being 10 to 20 per cent. In the present state of knowledge comment is scarcely possible, but if pellagra is, as some observers have suggested, a “deficiency disease,” it may be supposed that the transfused blood provides a temporary supply of the substance that is lacking; the patient is thus enabled to start along the road to recovery.
[67]
Appreciation of the dangers attending the practice of blood transfusion has varied greatly at different times. In the seventeenth century a happy ignorance took no account of them whatever. In the eighteenth century they were so greatly feared that transfusion fell into abeyance. In the nineteenth century it was realized that dangers existed, but they were imperfectly understood; when fatalities occurred, a partial knowledge explained them away more easily than our fuller knowledge can to-day, so that transfusion was practised in spite of them. At the beginning of the twentieth century, with the discovery of “blood groups,” it was thought that all danger had been eliminated. At the present time the pendulum is swinging back again, and the problem of the complete elimination of danger is proving more complex than it was thought to be a few years ago.
The chief dangers of blood transfusion are two-fold—that of introducing into the recipient a disease carried by the donor, and that due to the inherent properties of the donor’s blood which may interact in a serious manner with the blood of the recipient. The first of these dangers is obvious, and common sense will suggest what steps should be taken to avoid it. Danger of communicating disease is almost restricted to conditions in which an infective agent is actually circulating in some form in the blood. Inquiry will usually be enough to establish the possible presence in the prospective donor’s blood of an organism such as the malaria parasite. Nevertheless, a case has been recorded[68] by van Dijk, in which malaria was transmitted by injecting into a patient suffering from influenza some serum obtained from another patient who was supposed to be convalescent from influenza, but had been treated for malaria a few months earlier. Another case is reported by Bernheim, who transmitted a double infection of malaria—tertian and æstivo-autumnal—by means of a blood transfusion. Blood infections, such as those due to the exanthemata, may be avoided by the precaution of never employing a blood donor who shows any signs of present illness, even though a raised temperature be the only symptom. In certain cases, when, for instance, the prospective donor may be suffering from tuberculosis in some form or from gonorrhœa, the organism is extremely unlikely to be present in the blood in numbers sufficient to communicate disease. Nevertheless, on general principles, such donors should be eliminated if circumstances permit. The most subtle form of infection, the most dangerous, and the most difficult to eliminate, is syphilis. Definite cases have been recorded in which syphilis has been communicated by blood transfusion. In one instance recorded by Sydenstricker and by Bernheim a father was infected by blood taken from his son, who had refused beforehand to allow himself to be tested. Fortunately such occurrences are rare. Still rarer and still more curious is the transmission of horse asthma recorded by Ramirez. In this instance, in which the disease is to be regarded as a form of anaphylaxis, the patient had received an amount of serum sensitive to horse protein great enough to provide him with the corresponding symptoms for some time afterwards.
If the transfusion is being done at leisure, the donor’s blood must be tested for a positive Wassermann reaction. Even this test, however, has been known to fail, and since, in an emergency, the most careful inquiry, aided by a desire on the part of the donor to arrive at the truth, may reach an erroneous conclusion, the risk of infection with syphilis can never be completely eliminated. Since[69] reasonable care can make the danger a remote one, it need not hinder the performance of a transfusion any more than an occasional death under anæsthesia prevents the frequent use of general anæsthetics. The mere existence of such a danger is, however, an argument in favour of the general use of the “professional blood donor,” whose Wassermann reaction, personal history, and mode of life are well known to the practitioner; the previous use of his blood on perhaps more than one occasion, if unattended by any ill results, will give an added confidence. The tragedy of such a misfortune is so great that no precaution which can possibly be taken should be regarded as absurd.
The second danger present in the inherent qualities of the donor’s blood has been already alluded to in the historical sketch of the subject. Before the existence of the “blood groups” was realized, a number of fatalities due to an unexplained cause had occurred. Even after the existence of the groups had been demonstrated, the warning that resulted was apt to be disregarded, and it was not until still further fatalities due to this incompatibility of bloods had taken place that the very important nature of the discovery came to be understood. The chances are, on the whole, that the blood of any donor chosen at random will not prove fatal to a given recipient; nevertheless, it must frequently happen that the transfusion without being fatal will be wasted, or to some degree detrimental. It is therefore evident that the existence of blood groups must be seriously regarded, and it is necessary to enter into a detailed consideration of their relations to one another and the symptoms which they may produce. In the next chapters will be found a further description of their physiology and pathology and of the methods of testing for them.
It has long been known that if the blood of one species of animal is injected into the circulation of another species, the corpuscles of the foreign blood are at once destroyed, their contained hæmoglobin being set free. This process[70] of hæmolysis is under such circumstances rapid and complete, and hæmoglobin may appear in the urine in a short time. The precise nature of the reaction is obscure and need not be discussed here in detail. The present bearing of the phenomenon is the fact that a similar, or analogous, reaction may occur when the bloods of certain individuals are mixed with the bloods of certain others even of the same species. It was the observation of this fact that first led to the discovery of the so-called “blood groups” among human beings, and so to the partial elucidation of the cause of the previously unexplained fatalities following blood transfusion. In 1901 Landsteiner had detected the presence of hæmolysins and iso-hæmolysins in blood and classified three groups in human beings. In 1907 it was shown by Jansky that human beings may be divided into four groups, the blood of the members of each group having a certain definite relation to the blood of the other groups as determined by the manner of their interaction. The work was repeated and confirmed by Moss in 1910. The reaction takes place between the serum of one group and the corpuscles of the other groups, and is evidenced by the agglutination or hæmolysis of the corpuscles that are being acted upon. In the course of his researches Moss showed that hæmolysis, or the breaking up of the corpuscles, is always preceded by agglutination or the clumping together of the corpuscles. The process does not necessarily go as far as the destruction of the corpuscles, but may be arrested at the stage of agglutination. It may, on the other hand, be as rapid and complete as if the bloods belonged to different species, and the appearance of hæmoglobin in the urine may quickly give evidence of this.
The groups have been arbitrarily numbered, and it is now usual to refer to them by the Roman numerals I, II, III, and IV. According to the accepted convention, the reactions of these four groups are as follows:[5]
[71]
The corpuscles of Group I are agglutinated by the sera of II, III, IV. The corpuscles of Group II are agglutinated by the sera of III, IV. The corpuscles of Group III are agglutinated by the sera of II, IV. The corpuscles of Group IV are not agglutinated by any of the other groups.
On the other hand:
The serum of Group I agglutinates no other corpuscles. The serum of Group II agglutinates the corpuscles of Groups I, III. The serum of Group III agglutinates the corpuscles of Groups I, II. The serum of Group IV agglutinates the corpuscles of Groups I, II, III.
This may be represented more graphically by the following table, a + indicating agglutination, a – indicating no reaction:
| Serum | |||||
| I | II | III | IV | ||
| Corpuscles | I | – | + | + | + |
| II | – | – | + | + | |
| III | – | + | – | + | |
| IV | – | – | – | – | |
The active principle in the serum is called “agglutinin” or “hæmolysin,” according to the degree of the reaction, and the corpuscles are rendered sensitive to this by the[72] possession of an “iso-agglutinin” or “iso-hæmolysin.” Sometimes the corpuscles are said to have “agglutinophilic” properties. It may be stated, therefore, that the serum of Group I entirely lacks agglutinins, whereas the corpuscles of Group IV lack iso-agglutinins. All these terms, like the “amboceptors,” “receptors,” and “haptophores” of Ehrlich, are used to conceal ignorance rather than as an expression of knowledge, but, until more light has been shed upon the nature of the reactions, ignorance must be abbreviated.
It is now clear that the blood as a whole contains two sets of reactions which are independent. These properties reside in the serum and in the corpuscles respectively, and the reactions are complementary between Groups II and III, that is to say, the serum of each group agglutinates the corpuscles of the other. It will be seen from the table that the serum of Group I blood does not agglutinate the corpuscles of any of the other groups, and conversely the corpuscles of Group IV are not agglutinated by the serum of any of the other groups. Individuals of Groups I and IV have therefore been named “universal recipients” and “universal donors” respectively. This implies that if the recipient be found to belong to Group I, the blood of any donor may be transfused into his veins irrespective of his group, and that if the donor be of Group IV, his blood may be used for transfusion irrespective of the group of the recipient. These statements may be accepted as true in an emergency, but important reservations may have to be made under certain conditions.
It was at one time believed that the group reactions were clear-cut and absolute rather than relative. At the present time, however, the view is gaining ground that there may be some “over-lapping” of groups, that is to say, a serum may contain agglutinins which give a gross reaction with the corpuscles of one group and a reaction with another group so slight that it can be detected only with difficulty, or alternatively the recipient’s corpuscles[73] may give a definite and limited group reaction, while his serum may cause some agglutination in the blood of a theoretically compatible group. These properties have recently been termed “major” and “minor agglutinins” by Unger, who claims that the possible presence of minor agglutinins makes it advisable to test the recipient’s blood directly against the donor’s in every case. The term “universal donor” commonly applied to Group IV is, in fact, misleading. The blood of Group IV cannot be used indiscriminately with complete impunity. The groups are determined by the major agglutinins, and by these the ordinary gross reactions may be eliminated. Everyone who has used blood transfusions extensively has observed that slight reactions may occur after transfusion with a compatible blood, irrespective of the methods employed. Usually these reactions are slight, and do not in any way prejudice the benefits conferred by the transfusion, but they may become greatly accentuated in the later transfusions of a series, and it is probable that minor agglutinins may be developed in certain pathological conditions. Further reference to these phenomena will be made elsewhere (p. 93). In addition to this, it has been commonly observed that the intensity of the reaction varies greatly with the sera of different individuals of the same group. It has also been stated by Stansfeld that the agglutinating power of the serum of an individual may vary from time to time. As a rule the corpuscles of a person belonging to Group I are not agglutinated with equal rapidity or intensity by the sera of Groups II and III, but the meaning of this phenomenon has not been fully investigated.
A possible source of trouble will occur to anyone looking critically at the table of reactions, for it will be noticed that the serum of Group IV, the so-called “universal donors,” agglutinates the corpuscles of all the other groups. How does it come about, therefore, that the blood of this group may be given indiscriminately? The answer is to be[74] found in the fact that though the reaction takes place as shown in the table outside the body, nevertheless the serum of the transfused blood does not exert its agglutinating power in the body of the recipient. Several hypotheses have been advanced to account for this discrepancy, though no final explanation has yet been arrived at. In the first place it is possible that the agglutinating power of the serum is rendered ineffective by the dilution which it undergoes when it is mixed with the blood of the recipient. It has been shown, however, by Culpepper that agglutination takes place outside the body with serum diluted up to 1 : 150, a degree of dilution far greater than is ever obtained in a transfusion where the dilution in the patient’s circulation is usually no greater than 1 : 7. Secondly, it has been suggested that the transfused plasma meets with an excess of plasma containing protective or antihæmolytic properties. The evidence on this point is conflicting. Hektoen in 1907 was unable to demonstrate any such property in serum or plasma. Brem and Minot in 1916 both claimed to have demonstrated antihæmolytic properties in serum, and Minot added the observation that its concentration varies. Karsner in 1921 reported that he had failed to demonstrate anti-agglutinins in the blood. For the present, therefore, the point must remain undecided. Finally, it is possible that the agglutinins of the transfused plasma, meeting with an excess of agglutinable cells, are all absorbed without actually producing any agglutination. Whichever of these hypotheses be true, the fact remains that the blood of Group IV individuals may be given without serious effects in most ordinary cases in which transfusion is indicated.
It must not be inferred from the tabulated reactions that a transfusion with the blood of an incompatible group necessarily produces a fatal, or even a serious, result. If, for instance, an individual of Group II be transfused with blood of Group III, the corpuscles of the donor’s blood will certainly be rendered ineffective, being destroyed either at[75] once or in the course of a short time. But beyond this wastage of the transfused blood there may be no effects as shown by morbid symptoms in the recipient; he will merely not be benefited. There may, on the other hand, be an evident reaction in the recipient, the symptoms varying from slight discomfort to almost immediate death. It appears, therefore, that there is a gradation of toxicity between the bloods of incompatible groups, so that it may be justifiable owing to extreme urgency in certain cases to perform a transfusion without doing any preliminary tests on the bloods of donor and recipient. There is a good chance that the groups will be compatible; if, however, they be incompatible, there is still a good chance that the recipient will be no worse off than he was before the transfusion.
Even when the tests have been performed, it may still happen that through various causes a mistake has arisen. Owing to the inexperience of the operator or to staleness of the sera used in performing the test, an incompatible group may appear to be compatible. It is necessary, therefore, that everyone who performs a transfusion should be able to recognize the symptoms of a reaction as soon as it begins to appear, so that the transfusion may be at once discontinued. Sometimes the reaction between incompatible groups is so immediate and severe that death takes place almost at once. I did not myself perform any transfusions until after the period when blood-grouping tests had become a routine procedure, so that I have no personal experience of such unfortunate results. The symptoms may therefore best be described in the words of one who has several times witnessed the effects of an incompatible blood: “The clinical picture of these reactions is typical. They occur early, after the introduction of 50 cc. or 100 cc. of blood; the patient first complains of tingling pains shooting over the body, a fullness in the head, an oppressive feeling about the precordium, and, later, excruciating pain localized in the lumbar region. Slowly but perceptibly[76] the face becomes suffused a dark red to a cyanotic hue; respirations become somewhat laboured, and the pulse rate, at first slow, sometimes suddenly drops as many as from twenty to thirty beats a minute. The patient may lose consciousness for a few minutes. In one-half of our cases an urticarial eruption, generalized over the body, or limited to the face, appeared with these symptoms. Later the pulse may become very rapid and thready; the skin becomes cold and clammy, and the patient’s condition is indeed grave. In from fifteen minutes to an hour a chill occurs, followed by high fever, a temperature of 103° to 105°, and the patient may become delirious. Jaundice may appear later. The macroscopic appearance of hæmoglobinuria is almost constant.” (Peterson.)
In a fatal case recorded by other writers the chief symptom was hæmoglobinuria, which progressively increased until the functions of the kidney became so much interfered with by deposits of hæmoglobin or damaged corpuscles that the patient died with suppression of urine and all the signs of uræmia (25).
In other cases a slighter and transient hæmoglobinuria has been noticed, showing that some destruction of red cells has taken place without producing any further effects. This symptom is, of course, due to hæmolysis following reactions between the serum and corpuscles as explained above. The variation in degree of the reaction is to be partly explained by the fact that there are three possibilities: (1) The donor’s corpuscles may be hæmolysed by the recipient’s serum; this will result in the transient hæmoglobinuria and wastage of the transfused blood; (2) the recipient’s corpuscles may be hæmolysed by the donor’s serum, or (3) serum of each may hæmolyse the other’s corpuscles. Either of the latter events will be extremely serious. As already mentioned, hæmolysis is always preceded by agglutination, and it seems that the agglutination may be the more rapidly fatal of the two. It was probably this that was chiefly responsible for the suppression of urine[77] in the case referred to, and a case has been recorded in which it appeared to be the only cause of immediate death or, as an American writer expresses it, “sudden exitus took out, out of a clear sky,” owing to the presence of multiple emboli.
In addition to the evidence of hæmolysis the patient may exhibit the symptoms described above. Sometimes the urticarial rash has been accompanied by vomiting and headache. This group of symptoms suggests that the condition is analogous to the anaphylactic shock which may follow the intravenous injection of any foreign protein. The symptoms in a mild degree do occasionally follow the transfusion of blood which has been shown to belong to a compatible group, and it had been found to develop even to an alarming extent after the later transfusions, when a series was being given for a condition such as pernicious anæmia (34). In such cases, however, as is suggested elsewhere, this may, perhaps, be regarded as true anaphylactic shock. The symptoms which may accompany a first transfusion cannot be identical with this since true anaphylaxis must have been preceded by sensitization with a minimal dose of foreign protein introduced into the circulation.
It was formerly thought that possibly the products of hæmolysis were themselves toxic and capable of producing the symptoms described. This seems, however, to have been disproved by Bayliss, who has shown that in the dog and cat the hæmolysed blood of the same species is, with extremely rare exceptions, innocuous.
Another possible cause of similar symptoms is the sodium citrate used as an anticoagulant in one of the methods of transfusion subsequently to be described. But the symptoms, if due to this cause, will not be accompanied by any signs of hæmolysis, are usually not severe, and are always very transient. This will be referred to again later on.
The symptoms of incompatibility begin to be apparent[78] so quickly that the worst results can be avoided by the exercise of caution. If for any reason it has been necessary to use an untested blood donor, the first 100 cc. of blood should be injected very slowly. If no untoward symptoms result, the remainder of the blood can be injected with greater confidence. Little can be said as to the treatment of this condition, for prevention is far better than cure. When the symptoms have developed, the damage has been done, and cannot be undone. The ordinary measures for combating severe collapse may be used.
A lesser danger of transfusion is that of administering the blood too rapidly. Sometimes during a transfusion the patient complains of difficulty in breathing and a sensation of tightness in the chest; this should always be regarded as a warning that the blood must be given more slowly or perhaps that enough has been given and that the transfusion should be discontinued. Usually the symptom amounts to nothing more than discomfort, and will disappear if caution be exercised. The explanation is to be found in the too rapid filling of the venous side of an impaired circulation with overloading, and perhaps temporary dilatation, of the right side of the heart. I have never seen these symptoms occur to an alarming degree, but actual loss of consciousness with a very rapid and feeble pulse has been recorded by other writers. Directions as to the amount of blood which should be given and the rate at which it should be injected so that these symptoms may be avoided will be found under the description of methods given in a later chapter.
[79]
In the foregoing chapter the reactions between the blood groups and the morbid symptoms which may follow the injection of incompatible blood have been described. In the present chapter some account will be given of the more general physiology and pathology of the groups.
It seems to be clear that iso-agglutinins and iso-hæmolysins, that is to say, serum reactions among the individuals of a species, are to be found distributed widely through the animal kingdom. The phenomenon is, however, weak in operation compared with that found among human beings, and it is very much more difficult to demonstrate. The facts have not been investigated for very many species of animals.
Some of the earliest attempts to investigate the distribution of iso-agglutinins among animals were made by Hektoen in 1907. He tested the blood of rabbits, guinea-pigs, dogs, horses, and cattle; his results were negative in every case, but probably his technique was imperfect or an insufficient number of animals was tested. Grouping has been found among goats by Ehrlich. Ottenberg and others believe that they have demonstrated the existence of three groups among steers, and of four groups among rabbits. Von Dungern has shown that there are four groups among dogs. Agglutination reactions were found by Ingebrigtsen and by Ottenberg among cats, but they were not constant, and it was not found possible to distinguish any grouping. The same was found to be true of rats. I have not been able to discover any record of research upon iso-agglutinins[80] in birds or reptiles. The phenomenon of blood groups has a possible bearing on the success or failure of experimental transplantations of tissue, whether healthy or diseased, from one animal to another of the same species. From this point of view an investigation of the blood reactions among mice was carried out by B. R. G. Russell in the laboratories of the Imperial Cancer Research Fund, but he was unable to find any sort of grouping. Ingebrigtsen has made an attempt to correlate the results of the transplantation of arteries in cats with their serum reactions, but he was unable to do so. His results were equally bad whether iso-agglutinins were present or not. Nevertheless, it is highly probable that the success of tissue transplantation in man will be found to be largely dependent upon compatibility of blood groups in donor and recipient. The problem is one that cannot easily be investigated by experiment on animals, among which natural incompatibility is evidently much less well marked than it is in man. A method of overcoming this unsuitability is suggested by the experiments of Ottenberg and Thalimer. These observers, as already mentioned, found that in cats iso-agglutinins were present, though inconstant; on the other hand, iso-hæmolysins were seldom if ever found in normal cats, though they often appeared in the recipients of transfusions. Grafting experiments might therefore be preceded by transfusions designed to stimulate artificially incompatibility of the tissue fluids.
The incompatibility of blood is essentially a phenomenon which distinguishes different species of animals, since in no case can the blood of one species circulate unaltered in the blood-vessels of another kind of animal. This serological specificity may be in some way related to the sterility of one kind of animal with another, though not actually causing it, and so be merely an incidental phenomenon. It cannot be in any sense protective, since it never happens in the course of nature that blood is transferred from one animal to another. In the same way it is difficult to see[81] how there can be any biological “purpose” in similar differences between individuals of the same species, and, so far as is at present known, the possession of a particular group does not confer upon its owner any advantage over the individuals of other groups, such as a relatively greater immunity from disease, longevity, or fertility. It is quite clear that there is no connexion between incompatible blood groups and sterility between individuals.
An investigation of a possible relation between blood groups and disease has been begun by W. Alexander at St. Andrews University. In a preliminary communication concerning the blood groups found among fifty patients suffering from “malignant disease” of all forms, including leukæmia, he has found that there is a considerably higher proportion of Groups I and III than among healthy people. On the other hand, the groups are found in the normal proportions among people suffering from tuberculosis, syphilis, and tetanus. It would, however, be premature to assume that individuals of Groups I and III are more liable to suffer from “malignant disease” than other people, as the numbers tested are, at present, too small for definite conclusions to be formulated. Also it remains to be proved that the presence of malignant disease does not produce an alteration in the agglutinating reactions by which the groups are determined.
It seems probable that the differences between the groups have arisen incidentally in the evolution of mankind, possibly as the result of the parallel descent of two or more original stocks from different sources, which afterwards converged and mingled, with the production of serological hybrids. In view of this it is of interest to find that some investigation of the racial incidence of blood groups has already been carried out. On the Macedonian front during the war a large number of men of many different races were gathered together, and scientific advantage of this opportunity was taken by L. and H. Hirschfeld. The blood groups were determined in[82] approximately 8,000 individuals, including French, English, Italians, Germans, Austrians, Serbs, Greeks, Bulgarians, Arabs, Turks, Russians, Jews, Malagasies, Senegal Negroes, Annamese, and Indians. According to the results obtained by the Hirschfelds, the groups designated II and III show a definite variation in their distribution among different races. As will be seen hereafter, Group I is compounded of the two factors producing Groups II and III, while Group IV results from their absence. It is therefore necessary only to consider the incidence of Groups II and III in calculating the racial differences. For the statistical tables and diagrams the reader must be referred to the original paper published in 1919, but the results may be roughly summarized as follows. It was found that the factor producing Group II is prevalent among European peoples, whereas the factor producing Group III is characteristic of men from Asia and Africa. Thus the Group II factor was found in not less than 45 per cent. among most European peoples. It gradually diminishes in the countries lying between Asia and Central Europe, being present in Arabs 37 per cent., in Russians 37 per cent., in Jews 38 per cent. In Asiatics and Africans it falls considerably, being in Malagasies 30 per cent., in Negroes 27 per cent., in Annamese 29 per cent., in Indians 27 per cent. On the other hand, the factor producing Group III shows exactly the opposite variation. Among the English, the most Western people of Europe, it is rare, being found by these observers to be present in only 10 per cent.; it rises to 14 per cent. in French and Italians, to 18 per cent. in German Austrians, and to 20 per cent. in the Balkan peoples. In Africa and Asia the Group III factor rises considerably, being present in Malagasies 28 per cent., in Negroes 34 per cent., in Annamese 35 per cent., and in Indians 49 per cent.
We may still be far from elucidating the anthropological meaning of these facts, for the mingling of the hypothetical stocks of which mankind is made no doubt began in a[83] remote antiquity, and it is possible that a serologically pure race does not exist. The investigation, however, of the more isolated peoples might throw much light on the problems of anthropology.
Interesting as the wider questions may be, we are here more immediately concerned with the distribution of the blood groups amongst our own population. The percentages in which the four groups occur have been estimated by various observers, and, as will be readily understood from the foregoing remarks, the numbers show some variation. The approximate figures as worked out by three observers in America are as follows:
| Bernheim | Moss | Culpepper | ||
| (1,600 tests) | (5,000 tests) | |||
| I | 2 | 10 | 3 | per cent. |
| II | 40 | 40 | 38 | ” ” |
| III | 15 | 7 | 18 | ” ” |
| IV | 43 | 43 | 41 | ” ” |
The percentages found among the first hundred men whom I tested in the British Army in 1917 conformed almost exactly to the first of these series of figures, and they may be taken as an average result for Western peoples. It will now be seen upon what grounds it was stated in the last chapter that the chances were in favour of the blood of a donor chosen at random being compatible with that of the recipient. If the patient belong to Group II, then 83 per cent. of other bloods will be compatible. If he belong to Group III, 58 per cent. will be compatible. Only if he belong to Group IV will the chance in favour of compatibility fall below 50 per cent.
This statement of the facts concerning distribution of the blood groups will serve to emphasize the absolute necessity for the careful testing of a donor before his blood is used for transfusion. But, further than this, it is necessary to clear away several widely spread misappre[84]hensions as to the group relations between an infant and its mother and between the various members of a family. It has several times been stated in print that a mother’s blood must be compatible with that of her child, or sometimes that a baby has no blood group, so that it may be safely transfused with blood taken from its mother or its father without preliminary testing. On other occasions the statement has been made that the brother or sister of a patient is more likely than other people to belong to the same or a compatible blood group, so that untested blood may be transfused from one member of a family to another with little risk. Knowledge of the existence of blood groups has become somehow mixed up with vague popular beliefs concerning “affinities” and “blood relations.” Such confusions must, however, be dissipated, for none of these statements are more than partially true, and they may lead to a false sense of security and to disaster.
The assertion that an infant has no blood group was tested by the writer some time ago and shown to be false. On several occasions a newly born infant was tested and found to show well-marked agglutination reactions indicating Groups II or III as the case might be. Even in 1905 it had been shown by Martin that reactions could often be demonstrated between an infant’s corpuscles and the maternal serum, and sometimes between the infant’s serum and the maternal corpuscles. More recently (March 1920) the results of a full investigation into the reactions found in infants and children have been published by W. M. Happ in America. These researches began with the testing of blood from the umbilical cord, and this was seldom found to show the blood reactions as given by the adult. So far the statement quoted above was justified. It is even true that the serum of an infant’s blood will usually not give any reaction at birth or during the first month. The percentage in which it does give a reaction increases with the age of the child; after one year it is usually, and after two years always, established. On the other hand, the agglutination[85] reaction in the corpuscles appears before that in the serum, so that the grouping tested in this way may be present immediately after birth, as I found to be the case. It is possible that the grouping which first appears may afterwards be modified, but any change which occurs is always by the addition of factors and not by their subtraction; thus an apparent Group IV may become a Group II or III, or an apparent Group II or III may become a Group I. It is found that when a reaction is present in both the corpuscles and the serum, the group does not afterwards change. Happ’s conclusion, based on his investigations, was that it is unsafe to transfuse an infant with its mother’s blood without first making the usual tests, and the reasons for this will now be evident. In the first place an infant may be possessed of its final blood reactions very shortly after birth, and should therefore be treated in the same way as if it were an adult. In the second place, although its serum may be without agglutinating powers, so that transfused corpuscles will not be attacked, yet its corpuscles may be possessed of pronounced agglutinophilic properties, so that they may be seriously affected by the serum of transfused blood from an incompatible group. In the third place, as will presently be seen, it is by no means the rule that an infant should belong to the same group as its mother, whatever its blood reactions may be.
Another set of observations, leading to precisely the same conclusions, have been made by F. B. Chavasse of Liverpool. He terms the potential agglutination of the fœtal corpuscles by the mother’s serum, and of the maternal corpuscles by the serum of the fœtus, the “maternal threat” and the “fœtal threat” respectively, and states that there is no obvious relationship between the “fœtal threat” and eclampsia or the toxæmias of pregnancy. The inference is therefore justified that there is no transference of the agglutinating substances in either direction across the placental membranes. No chemical “immunity” is acquired, therefore, on either side, since the[86] protection is mechanical. This agrees with the fact observed by Happ that the mother’s milk contains the same agglutinins as the serum of her blood; but these do not have any deleterious effect upon the infant, and are therefore either not absorbed at all or are destroyed in the process of digestion.
The statement that the blood group of an infant is not necessarily the same as that of its mother can be amplified, for it has been found that blood groups are inherited on a definite plan, so that if the groups of the parents be known, certain predictions can be made as to the possible groups that may be found among their offspring. Many characters in animals and plants have been shown during the last twenty years to be transmitted according to the Mendelian plan of inheritance, but up to the present time very few normal characters in man have been isolated, and their manner of inheritance demonstrated, though a number of pathological conditions have been shown to conform to the theory. It is therefore of much interest to find that the inheritance of blood groups in man can be quite satisfactorily and consistently explained in Mendelian terms.
According to this theory, each quality in an organism which can be isolated and investigated independently of other qualities, is termed a “unit character,” and the appearance of each such unit character is determined by the presence of something called a “factor” in the sexual cells or “gametes,” male and female, by the union of which the individual is formed. Further, these unit characters are believed to occur in alternative pairs, and at first it was supposed that each alternative pair consisted of “dominant” and “recessive” characters, the second of which could only make its presence apparent in the individual if the dominant character were absent. Subsequently it was seen that the dominant and recessive characters need not necessarily consist of two positive, though opposite, qualities, but might better be regarded as consisting of the presence of a character and its absence. To use a classical[87] illustration of this view, sweet peas may be classified into tall peas and dwarf peas. At first the unit characters were taken to be tallness (dominant) and dwarfness (recessive). Later this idea was modified, and it was said that potentially all peas are dwarf, but to some is added a factor producing tallness, this factor being absent in those that are dwarf. To represent this idea more simply a conventional notation has been used, according to which the large letters of the alphabet indicate the presence, and the small letters the absence, of each factor.
In order to apply this theory to the case under consideration, it has been suggested that two pairs of factors are concerned:
A the presence of the character producing Group II.
a the absence of the character producing Group II.
B the presence of the character producing Group III.
b the absence of the character producing Group III.
Each pair of factors is transmitted independently of the other. Both A and B may be absent, in which case the individual belongs to Group IV; or both may be present, and in this case the individual gives the reactions of Group I.
It must be understood that the term “character producing Group II” is here used as a convenient way of expressing the obscure and probably complicated set of properties responsible for the reactions manifested by individuals of Group II. It includes not only the agglutinin or hæmolysin of the serum which reacts with corpuscles of Group III, but also the complementary iso-agglutinin or iso-hæmolysin by virtue of which the corpuscles react with serum of Group III.
The appearance of the different groups can now be further explained in terms of the Mendelian theory. According to the conception of the individual formulated by Mendel, each cell of the body contains an ingredient derived from each of the sexual cells or gametes which[88] united at the moment of fertilization of the ovum by the spermatozoon to form the individual. But when the adult in his or her turn forms sexual cells or gametes, these ingredients separate again, half the gametes containing one of the pair of factors, half containing the other. This process certainly takes place during the rearrangement of the nuclear substance or chromosomes at the cell divisions which result in the formation of the ripe sexual cells. It is called the “segregation of the gametes.”
In the present case the unit character producing Group II will be first considered. As already explained, the factors concerned may be called A and a, and the individual of Group II may be constituted by AA or Aa, and the gametes, therefore, may contain either A or a, but not both. The individuals resulting from the union of the gametes derived from Aa adults may then be constituted in three ways—AA, Aa, or aa. Similarly for the unit character producing Group III, the factors concerned may be called B and b, and the individual of this group may contain BB or Bb. The gametes then contain either B or b, and the individual resulting from their union may again be constituted in three ways—BB, Bb, or bb.
In computing the results, however, it must be remembered that most, or perhaps all, people are hybrids, so that both unit characters are present simultaneously, and all the factors must be taken into account. It is easily seen that the gametes derived from a hybrid individual must contain one of the following combinations:
AB, Ab, aB, or ab,
and consequently the individuals formed from them must have one of the following constitutions:
AB—Ab, Ab—aB, aB—ab, ab—ab, AB—AB,
AB—aB, Ab—ab, aB—aB,
AB—ab, Ab—Ab.
This includes all the possible combinations that can result from the chance union of the gametes, and it is now clear[89] which blood groups result from which combinations, if it be remembered that
| A | is dominant to | a, |
| B | ” ” ” | b, |
and that
| Group I | results from the presence of | both A and B. |
| ” II | ” ” ” ” ” | A only. |
| ” III | ” ” ” ” ” | B ” |
| ” IV | ” ” ” absence ” | both A and B. |
| Thus Group I | may be constituted by | AB—AB. |
| AB—aB. | ||
| AB—Ab. | ||
| AB—ab. | ||
| Ab—aB. | ||
| Group II | may be constituted by | Ab—Ab. |
| Ab—ab. | ||
| ” III | ” ” ” ” | ab—aB. |
| aB—aB. | ||
| ” IV | ” ” ” ” | ab—ab. |
It now becomes evident what offspring may result from the union of parents who have any of the above constitutions. Thus parents both of Group I may have offspring belonging to any group according to which of the five possible constitutions they possess. If the union be represented by
AB—AB × AB—AB,
then only offspring of Group I can result, since every gamete contains both A and B. The other possibilities may be worked out by the reader if he desire.
Similarly, a union of Groups I × II, I × III, or II × III may produce any of the groups, definite limitations being imposed by the detailed constitution of the parents. On the other hand, the remaining group unions that are possible can only produce a more limited variety of offspring. Thus II × II or II × IV can only produce[90] Groups II or IV; III × III or III × IV can only produce Groups III or IV; IV × IV can only produce Group IV.
The Mendelian theory of inheritance in general has been subjected to a prolonged and widely ramifying series of tests, and it seems in the present state of knowledge to present a satisfactory and consistent explanation of the facts. For a more extended account of it the reader must be referred to the standard works on the subject.[6] As regards its application to the present case, the test of actual experiment has not yet been carried out on a large scale. A series of observations has, however, been published by J. R. Learmonth, who, taking forty families at random, determined the blood groups of both parents and the children in each family. In this way he tested most of the possible group matings, and, with a single exception, the group inheritance conformed to the theory as set out above. Additional confirmation of the truth of the theory is afforded by the pedigree given on the page opposite. I have recently collected this pedigree, which includes fifty-nine individuals belonging to four generations, and it has not been published before. It will give, perhaps, a more graphic representation of the facts than has been conveyed by the brief summary contained in the foregoing pages. It does not show any variation from the results that were to be anticipated according to the theory.
The exceptional result obtained by Learmonth in one of his forty families serves to emphasize the clarity of the theoretical considerations. In this family parents both belonging to Group IV had a child showing the reactions of Group I. There are three possible explanations of this:
(1) The observations were at fault.
(2) The putative father was not the real father.
(3) The Mendelian theory of inheritance is wrong.
The Mendelian theory is established on so firm a basis that, in the absence of more numerous exceptions, (3) may be rejected. There is no reason for supposing that the observations were inaccurate, and we are therefore brought to the conclusion that in such a case the child is illegitimate.
[91]
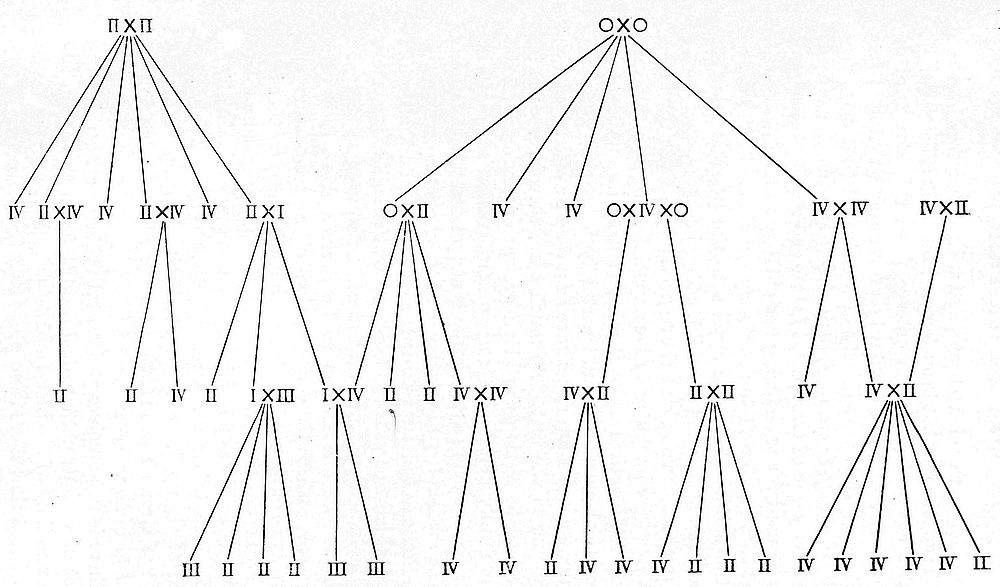
[92]
The conclusions which emerge from this structure of theory and fact are obviously of very great clinical importance. It is now clearly demonstrated that a mother belonging, say, to Group I, may give birth to a child belonging to any one of Groups I, II, III, or IV; her blood may not be used for transfusing her child without a grave risk that the “maternal threat” may culminate in the death of the child. The same applies to the possible relations between a father and his child. Two brothers, again, may belong to Groups II and III respectively. Even the blood of twins may be mutually incompatible, except in the rare case of “identical twins,” who, it may be supposed on theoretical grounds, would certainly belong to the same group, though I am not aware of a case in which this has been put to the test. As much care, therefore, must be exercised in testing the blood groups of members of the same family before performing a transfusion as would be taken before using a donor who is not related to the patient.
The medico-legal importance of the facts concerning the inheritance of blood groups is also evident, and, although this test has not yet been used as a test of legitimacy, there can be little doubt but that it will be so used in the near future. The information to be derived from it is of a negative rather than a positive character. Thus the occurrence of Group III blood in a child whose mother is of Group II and putative father of Group I cannot be taken as a proof either of legitimacy or the reverse. But if, as in Learmonth’s case, parents both of Group IV have a child of Group I, or if parents both of Group II have a child of Group I or III, then this may be taken as a proof of illegitimacy.
There is not much experimental evidence concerning the effect of various pathological conditions on the agglutination reactions of the blood and serum. It has already been mentioned that there is no proof that the possession of any[93] particular blood group confers upon its owner any special immunity from, or liability to, disease. The numbers, investigated by Alexander in the communication referred to on p. 81, are too small for the observation to be of much value; it is also necessary, as a preliminary to any such research, to demonstrate that there is no abnormal alteration in the reactions of the blood of these patients. It is probable, indeed, that evidence of this alteration in malignant disease already exists, for a reference to it is to be found in Kolmer’s work on serum-therapy,[7] but I have been unable to find a record of the investigation.
I possess, on the other hand, evidence that an alteration may take place in some other diseases, such as pernicious anæmia and familial, or acholuric, jaundice. Evidence for the former was provided recently by a patient whose condition was typical, clinically, of the last stages of the disease. Her corpuscles, tested with stock sera, belonged to Group II, but her serum, tested directly with the corpuscles of prospective donors known to belong to Group IV, agglutinated these vigorously, so that a transfusion could not safely be performed. The same phenomenon has been found by other observers. In acholuric jaundice there is a progressive destruction of red corpuscles in the patient’s circulation. This appears to be connected in some way with an abnormal functioning of the greatly enlarged spleen, since the destruction of corpuscles ceases almost at once when this organ is removed. There seems to be, in addition, an alteration in the blood reactions. In a case which I tested recently, the patient’s corpuscles were quickly agglutinated by serum of Group III, and he therefore nominally belonged to Group II. His serum, however, when separated and tested against other bloods of known[94] groups gave, in addition to a rapid agglutination of corpuscles belonging to Group III, a definite, though slower, agglutination of corpuscles belonging to Groups II and IV, showing that it had acquired abnormal properties.
It is possible that there are similar alterations of reactions in other pathological conditions. The instances mentioned above suggest that the serum is affected rather than the corpuscles, but further investigations are needed. It is an observed fact that blood outside the body soon develops the property of auto-hæmolysis. If blood is drawn from a vein, put into a test-tube, and allowed to clot, then after twenty-four hours or more the serum which has separated from the clot begins to be tinged with hæmoglobin, even though it has remained absolutely sterile. It appears, therefore, that the serum develops a hæmolysin and the corpuscles the corresponding iso-hæmolysin, the interaction of which results in the breaking up of corpuscles. If this process takes place in normal blood outside the body, it would not be surprising to find that it may also occur abnormally inside the body. This actually happens in the condition known as paroxysmal hæmoglobinuria. The pathology of the disease is obscure, but it seems that a hæmolysin develops in the serum as the result of cooling in the extremities and hæmolysis takes place when the cooled serum is again warmed by being restored to the general circulation. The presence of this hæmolysin in addition to the normal hæmolysins has been demonstrated by Moss. It is possible that a similar though less acute change takes place in acholuric jaundice. Blood transfusion, therefore, is not likely to be efficacious in such conditions, since the transfused corpuscles may be destroyed whatever the apparent blood group of the patient. Some of the facts of auto-hæmolysis have been recently investigated by Bond, but it is not necessary to give the details here. He concludes that the development of auto-hæmolysins, which are non-specific and independent of the specific hæmolysins of the blood groups, has a[95] biological significance in the history of the red corpuscle, and is a product of ageing. The biochemistry, however, of the process remains at present entirely unknown.
The necessity for careful blood grouping in every case before performing a transfusion has now been sufficiently emphasized, but before proceeding to the description of the methods of choosing a donor and of grouping, a possible danger must be mentioned which may arise even when the blood groups are known. In the preceding chapters references were made to the effects which have been observed to follow repeated transfusions given in the treatment of a condition such as pernicious anæmia. In such cases, although the groups were ascertained, and the bloods were also tested directly against one another without any incompatibility being detected, yet when the third or fourth transfusion was given, symptoms of toxæmia followed, sometimes with hæmolysis. The death of the patient has even been hastened in this way. A very striking instance of this phenomenon, which has been recently reported (278), will serve to bring home the reality of the danger. A boy was transfused by the citrate method with blood from his father, and this was followed only by a mild febrile reaction such as is often observed. Eighteen days later a second transfusion with blood from the same donor was performed, and after 150 cc. had been given, a severe reaction resulted, which was followed later by pronounced hæmoglobinuria. In this case the bloods of donor and recipient had been tested against one another directly, but this was not repeated, and the groups were not ascertained until afterwards. Probably there was some error in the original test, for it afterwards appeared that the boy belonged to Group I and his father to Group III, so that there should have been agglutination of the boy’s corpuscles by his father’s serum outside the body. Nevertheless, Group I individuals have been called the “universal recipients,” and no ill effects are usually observed whatever blood be used for transfusing them. In the other cases[96] already mentioned a reaction followed the later transfusions, even when the donor and recipient belonged to the same group. It appears that by repeated transfusions the recipient becomes as it were sensitized to the blood of another individual even of the same group, and consequently great caution must be used in giving the later transfusions of a series. Some light is thrown on this question by the observations of Ottenberg, already referred to, concerning the artificial production of iso-hæmolysins in cats. In these animals iso-agglutinins are found, but iso-hæmolysins seldom or never. The reaction is, however, found to become hæmolytic in the recipients of transfusions, and it is then selective. It seems, therefore, that the group reactions may not be as clearly defined as was at one time supposed. Probably there are slight incompatibilities of an unknown nature between individuals of the same or compatible groups. These are very seldom of any consequence in a first transfusion, but become accentuated as the result of “sensitization,” and in later transfusions have a pronounced influence. This “over-lapping” of groups has been mentioned on another page. It must not be supposed that any untoward results follow repeated transfusions as a general rule, for usually no such effect is observed. In order, however, to minimize the risk, it may be suggested that the following precautions should be taken: (1) The donor should be actually of the same group as the recipient, and not merely of a theoretically compatible group; a patient, for instance, of Group II should receive blood of Group II rather than of Group IV. (2) The same donor should not be used for the later transfusions of a series, on the grounds that the sensitization appears to be an individual rather than a group phenomenon. (3) In performing the later transfusions, the blood should be given at first very slowly, so that it may be discontinued at the first appearance of any signs of a reaction.
[97]
The physiology of blood groups having been examined, the principles governing the choice of a blood donor can be more readily understood. It is evident that this choice is determined largely by blood groups, and in the present chapter therefore the clinical methods of testing for the groups will be described.
Before, however, the bloods can be tested, a willing donor must be found, and this is not always an easy matter. During the war, even when transfusion was being practised on a large scale, there was never any difficulty in finding volunteers among the men that were more lightly wounded. In addition to the genuine and ready response which many men would make at once to a call for help in a matter of life and death, there was the glamour of novelty and the feeling of satisfaction following an act of conscious heroism—for such the sacrifice of blood was held to be, the days having long been forgotten when as much blood was “let” in the treatment of almost any ailment. In the Expeditionary Force, too, the unofficial reward of a fortnight’s leave in England proved a potent inducement, and the rejection of a volunteer on the ground of incompatibility was regarded almost as an injustice or as a reflection upon the physical condition of the candidate. In civilian life, however, such inducements cannot be held out, and it will be found that many a man “does not like the idea” of parting with a pint of blood, even though the sacrifice may save another’s life. Often, however, a near relative of the patient may happen to be willing and suitable, or, failing[98] this, in a hospital ward there will usually be some young man who has been admitted for a slight operation, such as the radical cure of a hernia, and will accede to a request for blood if the procedure, its object, and its harmlessness to himself be briefly explained. Notoriety is fortunately seldom a motive for volunteering, and though paragraphs have occasionally appeared in the daily press with headings such as “Police Inspector’s Sacrifice,” this has probably not been done by the donor’s own wish. It is, after all, natural that to the mind of a layman the giving to another of so personal a possession as his blood should seem to be an act of heroism, and it is also natural that occasionally a man should feel some repugnance to taking part in a strange performance which he but dimly understands. To the young, on the other hand, the procedure may appeal by its faint flavour of adventure.
Occasionally during the last two years advertisements for blood donors have appeared in newspapers, probably not in vain. If the demand for blood donors becomes greater than it has been as yet, it will certainly result in the creation of a class of “professional blood donors,” who already exist in some numbers in the United States of America, where blood transfusion is a more widely recognized form of therapeutics than it is in this country. These professionals have even formed a Trade Union, so that as high a fee as possible may be obtained from those who need their blood. Apart from this, some of the advantages of having these professionals available have already been explained in the chapter on the dangers of blood transfusion. It is evident that certain sources of danger can be eliminated in advance, and in an emergency it is obviously better to have donors of known groups available, so that no time is lost in testing the prospective donors of whom several in succession may be found unsuitable. Probably it will be easier for practitioners to arrange for such professionals to be available at the shortest notice than for necessary arrangements to be made[99] in a hospital. Even in large institutions it is usually difficult for any of the men employed in them to be spared from their work for twenty-four hours, so that, although suitable men of known groups are always within call, it may be impossible to use them. This, however, is not the place to discuss the organization that is necessary to make a blood transfusion a really efficient form of emergency treatment in a hospital. It may merely be observed that in every hospital it should be possible to give a blood transfusion to a patient suffering from urgent hæmorrhage within fifteen minutes of his arrival on the premises.
Whether the donor be a “professional” or an “amateur,” it may be useful to mention a few points to be observed in choosing him. There can be no doubt that the most satisfactory individuals for the purpose are young men between the ages of eighteen and twenty-five. The younger the donor, the less likely is he to be suffering from certain of the diseases mentioned in the chapter on the dangers, the less will be the immediate effect of the withdrawal of circulating fluid, and the more quickly will he recuperate from the loss of blood.
It must not be supposed, however, that the withdrawal of even 1,000 cc. of blood will usually have an appreciable effect upon a healthy man. It is impossible to predict from the donor’s appearance what immediate effect the loss of blood will have upon him. It sometimes happens that the most robust-looking individual becomes faint after losing a few hundred cubic centimetres, whereas another, to all appearances pallid and much less satisfactory, will not evince the slightest discomfort from the loss of 750 cc. or even more. Normally a man should be able, by his physiological mechanisms, to compensate reflexly and at once for the removal of this amount of fluid from his circulation. In any case, the worst effect that is seen in a well-chosen donor is a transient faintness; it is usually wise to keep him on his back for two or three hours after the operation, and he should not, if it can be avoided,[100] return to his work on the same day. During the late war a medical officer of my own acquaintance gave 750 cc. of blood for a severely wounded friend and continued his arduous duties as Surgical Specialist in a Casualty Clearing Station immediately afterwards. In this case, however, the donor was solely responsible for his own welfare; usually this responsibility rests upon another, and greater care must be exercised. The effect, indeed, of a transfusion upon the donor seems to depend more upon psychological than upon physiological factors. A nervous and excitable donor is more likely to suffer than one who approaches the operation without apprehension. This is another point in favour of employing a professional donor, who soon becomes familiar with the whole procedure and will lose all symptoms of fear.
The same considerations may be applied to the use of women as blood donors. In them the spirit of self-sacrifice is commonly more highly developed than it is in men, and some of the most eager donors will be found among them. The disability of nervousness will, however, occur more often in women, and another consideration of importance is that the veins of a woman are usually much less easily accessible than those of a man. Not only is the abundant subcutaneous fat an impediment in women, but usually the superficial veins are all of small size. The method of choice for performing a blood transfusion will be presently described, and it will then be seen that the operation is easier and that much less damage is inflicted on the donor if a large superficial vein can be tapped. In women this will very often be difficult or even impossible. In general, therefore, it may be stated that the use of women as blood donors is to be avoided. The fallacies concerning the indiscriminate transfusion of an infant with its mother’s blood and of any patient with the blood of a near relation have already been explained.
[101]
Reference to the table of blood reactions given on p. 71 will show that in order to discover the blood group of any individual it is only necessary to test his corpuscles against the serum of Groups II and III. These reactions may be recapitulated as follows:
(i) If he be Group I, his corpuscles will be agglutinated by the serum of Groups II and III.
(ii) If he be Group II, his corpuscles will be agglutinated by the serum of Group III only.
(iii) If he be Group III, his corpuscles will be agglutinated by the serum of Group II only.
(iv) If he be Group IV, his corpuscles will be agglutinated by neither serum.
Only the serum, therefore, collected from people known to belong to Groups II and III need be kept in stock. This can generally be obtained from the Lister Institute, and if kept sterile will retain its agglutinating properties for some months, but under no circumstances should serum more than six months old be used, since the consequences of a failure to agglutinate may be very serious. Nevertheless, the agglutinins contained in serum are very resistant to physical and chemical changes in their environment. Dried serum has been successfully used for testing purposes, and Culpepper has shown that the reactions are not interfered with by cold or by heat until actual coagulation of the serum takes place. Bacterial contamination does not affect the reactions, so that the serum is still active even when putrid. Various methods have been used for preserving the serum. Its properties are not affected by the addition of dilute cresol (1 : 250) or of chloroform.
In the absence of any stock sera, the agglutinating test may be applied directly. A few cubic centimetres of blood are taken from the patient, and the serum as soon as it has[102] separated is tested against the corpuscles of the prospective donor. If agglutination occurs, this donor is at once excluded. If no agglutination occurs, he is either of the same group as the patient or belongs to a compatible group. Supposing that a donor actually of the same group as the patient is wanted, then the reverse test must be performed in addition, that is to say, the corpuscles of the patient must be tested against the serum of the donor. If both tests are negative, then donor and patient are proved to be of the same group. The method of direct test cannot be applied in an emergency owing to the loss of time involved; it is better, therefore, that anyone who intends to be ready to perform a blood transfusion should always have serum of Groups II and III immediately available.
The collection of stock sera is not a matter of any difficulty. With strict aseptic precautions 20 cc. of blood are withdrawn in a syringe from persons known to belong to Groups II and III; the bloods are put into a sterile test-tube and allowed to clot. As soon as the serum has separated it is drawn up into sterile glass bulbs of suitable capacity, which are sealed off at each end. The most convenient form of storage for actual use is a capillary glass tube sealed at each end. Each tube may be made to hold a single drop, which is the amount used for a test. There is then no wastage of serum, and no chance of contaminating the remaining stock. When the blood has been withdrawn and has clotted, the complete settling of the corpuscles can be hastened by the use of the centrifuge. If the serum be left in contact with the corpuscles for more than twelve hours, some auto-hæmolysis may take place, so that the serum will become tinged with hæmoglobin. It is exceedingly important that the two stock sera should not become confused, and this may easily happen unless each tube has some distinguishing mark.
The methods of testing for blood groups have been simplified by successive observers since the existence of the groups was first demonstrated in 1907. Moss used an[103] elaborate technique such as was essential for putting a new discovery upon a secure scientific basis. In order to obtain a suspension of corpuscles, blood was drawn into a syringe containing a solution of sodium citrate to prevent clotting. The corpuscles were collected by means of the centrifuge, and were thoroughly washed twice in normal saline solution so that they were finally collected free from serum and from citrate. Serum was collected in the manner already described. A series of small tubes was then filled with equal quantities of serum and the suspension of corpuscles, and was incubated for two hours at 37·5° C. At the end of this time observations were made and again after the tubes had stood for twelve hours in an ice chest. Varying degrees of agglutination and hæmolysis were then accurately recorded, and far-reaching results were obtained.
Later workers had the advantage of using stock sera belonging to known groups, so that the number of observations to be made was very greatly reduced. Brem introduced in 1916 a method of testing in which he mixed the serum and suspension of washed corpuscles in very small quantities on a coverslip, which was inverted over an ordinary cell slide rimmed with petroleum jelly. The results could then be observed macroscopically or under the microscope, and the presence or absence of agglutination could be determined within fifteen minutes. The detection of hæmolysis by the hanging drop method requires that the cells should be incubated and observed at intervals for several hours, but it is not always easy to see the disintegrated corpuscles unless the process has taken place extensively. The diagram on p. 105 gives in a tabulated form some idea of the appearances presented by the corpuscles of the different groups when mixed with the stock sera and observed in a hanging drop under a microscope. Agglutination must be distinguished from the formation of rouleaux, which may be seen in any of the mixtures.
[104]
For scientific purposes these very careful tests are necessary, but it seems to be clear that for clinical purposes a much rougher and quicker test is adequate. In the clinical determination of blood groups it is superfluous to carry the test to the point of watching for hæmolysis, for it is upon the presence of agglutinins in the serum and the corresponding iso-agglutinins in the corpuscles that the determination of the groups depends. Further, no error is introduced by neglecting the hæmolysis, since it has been shown that hæmolysis is invariably preceded by agglutination. It is the occurrence of agglutination therefore that is of prime clinical importance. If that is excluded, hæmolysis is necessarily excluded also, and the prolonging of the test is seen to be only of academic interest. In the methods described above the corpuscles were always tested in the form of a washed suspension. This precaution was taken on the supposition that the presence of any of the serum belonging to the corpuscles might interfere with the reaction. If, however, the amount of this serum be small relatively to the amount of the test serum, then no such interference takes place.
[105]
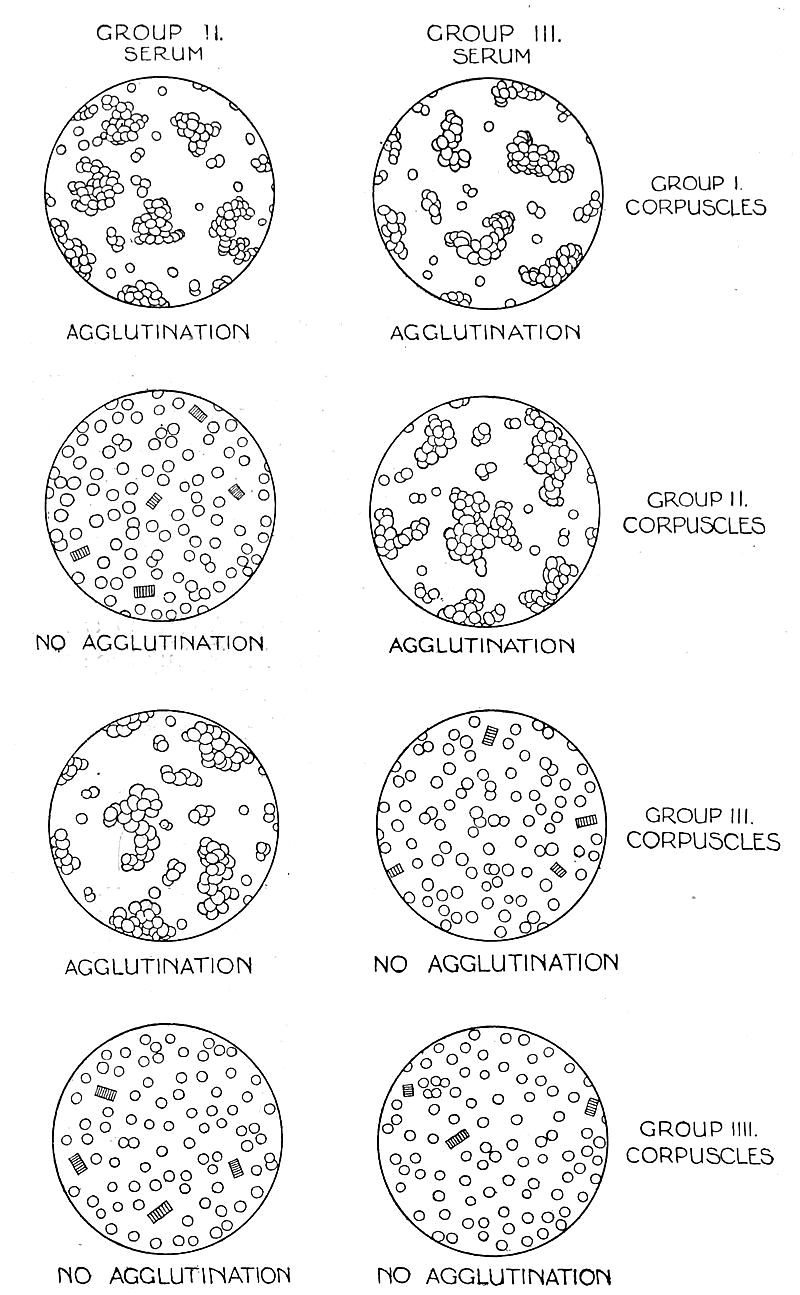
The ordinary clinical method of testing may therefore be greatly simplified, and the one commonly used at the present time is as follows: A single drop of each of the stock sera is placed on two glass slides, or, better, side by side upon a white glazed tile or plate, the numbers of the groups, II and III, being written above the respective drops. The lobe of the ear of the person to be tested is then washed with ether and pricked with a sterile surgical needle. A small quantity of the blood which exudes is taken up on the end of a blunt metal or glass rod, and is intimately mixed with the drop of serum under the number II. The end of the rod is then carefully wiped clean, and a similar small quantity of blood is mixed with the drop of serum marked III. The amount of blood to be used should not be so great as to make the drop of too deep a colour, which may interfere with observation of the reaction, but [106]it should be enough to impart to it a very definite red tint. The slide or tile is then gently rocked, so that some slight movement is imparted to the drops, which are at the same time closely watched in a good light. The agglutinating reaction is readily seen with the naked eye, especially against the white background provided by the tile. If the serum be properly active, the agglutination of the corpuscles begins to be apparent as a definite granular appearance resembling brick dust within a minute of mixing. With a little practice this appearance is easily recognized, but it must be distinguished from the appearance produced by a mechanical gravitation of the corpuscles towards the centre of the drop. If agglutination is taking place, the granulation appears simultaneously throughout the drop, and not only in the centre. With an active serum the process may proceed rapidly, so that in less than five minutes the corpuscles have been aggregated into a few irregular masses; often it stops short of this, but the drop presents, nevertheless, a coarsely granular appearance which is quite unmistakable. If no granulation can be seen at the end of five minutes, it can be assumed that the test is negative for the serum of that group, and the group of the corpuscles may be deduced upon the principles already explained.
The test carried out in this way is admittedly not susceptible of the same finesse as if it were done with the assistance of the hanging drop, the incubator, and the microscope; nevertheless, my own experience in a large number of cases has shown that, clinically, this test may be relied upon, and the same view has been expressed by other writers on the subject. Very seldom is there any doubt as to the presence or absence of agglutination. When doubt exists, it is easy to repeat the test and obtain a confirmation of the result. It may perhaps be urged that this test is quite insufficient for eliminating the slighter degrees of incompatibility which have produced serious results when the transfusion has been repeated[107] several times. But in the cases reported, the blood that was used had not shown any agglutination even when most carefully observed under the microscope. It seems, therefore, that the results were probably due to another factor, as already suggested (see p. 57), which the more elaborate test failed to eliminate. The efficiency of the rapid test is therefore not invalidated. It is, nevertheless, in the present state of knowledge, a wise precaution to perform the direct test between patient and donor in addition to the group test when circumstances permit. It is essential when the patient is suffering from any form of blood disease. It is unnecessary when the transfusion is to be performed as a life-saving operation in hæmorrhage or shock.
[108]
Some reference has already been made in the first chapter to the rapid development in recent years of the technique of performing a blood transfusion. The earlier operators, owing to the difficulties introduced by the coagulation of blood outside the body, were constrained to make use of some method of direct transfusion, the blood flowing directly from an artery of the donor into the patient’s veins. This has now been largely replaced by one of the methods of indirect transfusion, the blood being withdrawn from the donor into a vessel in which clotting is delayed or prevented, and then injected or allowed to run into the patient’s circulation.
Direct Transfusion.—The obvious method of performing a direct transfusion is by making an end-to-end anastomosis between an artery of the donor and a vein of the recipient. The most readily accessible artery is the radial at the wrist, and this is indeed almost the only artery that is available. The most accessible vein is the median basilic or the median cephalic at the elbow. The operation of end-to-end anastomosis, using an artery of so small a calibre as the radial artery at the wrist is usually found to be, is one of great technical difficulty; this effectually prevented transfusion from being used at all frequently. A modification has been used by Sauerbruch and others, in which the end of the radial artery is drawn into the lumen of the vein through a slit in its wall. A suture is passed through the radial artery close to its cut end, and the needle is then passed through the slit in the vein and[109] out again through the wall of the vein an inch or so higher up. Traction on the suture then pulls the artery into the vein. The artery has meanwhile been temporarily occluded by a clip, which is removed when the artery is inside the vein, so that the blood can then flow from one to the other. This is easier to do than the anastomosis, but, in addition to the other objections to direct transfusion to be mentioned presently, the difficulty occurs of occlusion of the artery by the physiological process of inversion of its coats at the cut end. This is likely to happen before much blood has passed, so that apparent success at first is often not maintained. Sauerbruch claimed that the amount of blood that had passed could be estimated by measuring the time taken for 1 cc. of blood to flow from the artery before it was introduced into the vein; but there is no proof that the rate of flow remains constant.
If direct transfusion be desired, there can be no doubt that Crile’s method, introduced some fifteen years ago, is the best to employ. After much patient work Crile perfected a method of anastomosis which ensures that no occlusion of the vessels can take place at the site of junction. This depends on the use of a short silver tube, through which the end of the artery is threaded. The artery is then pulled back again outside the tube in the form of a cuff and fixed in position. The end of the artery has thus been made rigid, and over this the vein is pulled in its turn and fixed by a ligature. A watertight junction is thus made, and blood can flow through it without interruption—unless clotting takes place in the vessels as the result of handling and injury to their walls. This method has been extensively used in America, and it was the first to render the operation of transfusion a comparatively popular one.
Various other devices for achieving the same result have been elaborated by other workers, and attention may be drawn to those of Elsberg and Bernheim, both of which are described in the book by the latter on “Blood Transfusion.” During the war a simpler method was introduced[110] by Colonel Andrew Fullerton, who, working at a Base Hospital in France, found that he could get good results by employing a thin rubber tube with a small silver cannula at either end. The apparatus was first coated on the inside with a thin layer of paraffin wax, in order to discourage clotting within the tube, and the cannulæ were introduced into the donor’s artery and the recipient’s vein respectively. The blood could then flow freely from one to the other. The fact that blood was being transmitted was taken to be proved by the visible pulsation of the thin rubber connecting-tube synchronously with the arterial pulsations. The disappearance of this was assumed to be evidence that clotting had occurred. This method was described by Colonel Fullerton to the surgeons working at the Casualty Clearing Stations, where blood transfusion was likely to be of most service, but it was never used extensively. The coating of the inside of the tube with paraffin is in itself an operation of some difficulty. Under conditions in which any loss of time could not be permitted, success by this method was not attained with sufficient certainty, and it was shortly afterwards replaced by the more satisfactory methods described below. The most recent work on direct transfusion has been done by J. M. Graham at Edinburgh, who has however reached the conclusion that the technique is always more difficult than that of indirect transfusion.
It can easily be seen, therefore, that all the known methods of direct blood transfusion present great technical difficulty, which renders the method unsuitable for general use. There are, in addition, certain other objections to it of an obvious nature. It is, in the first place, impossible to measure the amount of blood which has passed from the donor to the recipient. Sometimes an indication may be obtained from the evident improvement in the condition of the patient, accompanied by the signs of loss of blood in the donor. More often clotting takes place, unknown to the operator, at some point, with the result that blood[111] ceases to pass a considerable time before the end of the operation, and the patient has consequently received very much less blood than is supposed. It has been claimed by Libman and Ottenberg that the amount of blood transferred may be estimated by weighing the donor before and after the operation. This presupposes that a very accurate weighing machine is easily available, which usually is not the case.
A second objection is the extent of the injury which is necessarily inflicted on the donor. His radial artery must be exposed through an incision of considerable length, and must be ligatured at the conclusion of the process. The operation becomes, therefore, a matter of some moment to the donor, who will be permanently scarred, and can under no circumstances be used for transfusion more than twice.
A third objection is that the transfusion cannot be done with due regard to the condition of the patient. A delicate and difficult operation has to be performed with the donor and recipient lying side by side, their arms close together. It is therefore almost imperative that both should be on operating-tables of a convenient height. Often, however, with an exsanguinated patient it is very important that he should not be moved from his bed, but as a bedside operation direct transfusion becomes difficult indeed!
A final objection is that in some people the radial artery is of very small calibre, so that when all preparations have been made, and the artery exposed, it is found to be quite impossible to proceed. Another element of uncertainty is thus introduced.
There is, therefore, little to be said in favour of direct transfusion, and much to be urged against it. This method has, indeed, in my own opinion, come to be of historical interest only. For this reason the different methods have only been very briefly described. For more detailed information, reference must be made to the various original communications, which will be found in the Bibliography.
Indirect Transfusion.—The methods of indirect[112] transfusion may be divided into those which depend upon the use of an anticoagulant mixed with the blood and those in which the blood is given unaltered. The technique of either process is simple compared with that of direct transfusion, though any method which makes use of whole blood can never be quite as free from uncertainty or difficulty as one which introduces the use of an anticoagulant. If the blood is prevented from clotting, the chief cause of failure in performing blood transfusions is removed. With any whole-blood method of transfusion speed is exceedingly important, frequent practice is a very great advantage, and it is essential, as with direct transfusion, that the donor and recipient should be in close proximity to one another, if not actually side by side.
On the other hand, the use of an anticoagulant renders speed and frequent practice of less account. The blood can be drawn, and can then be put on one side until the best moment for giving it has arrived. Due regard may be had to the patient’s condition, since the blood can be carried about and can be given at leisure to the patient in his bed without disturbing him and almost without his knowing it. The donor, too, is not exposed to the mental shock of lying for some time side by side with a patient who may be in extremis, or may even expire during the operation.
There are, however, those who consider that the use of whole blood, instead of blood which has been chemically treated, has advantages which outweigh the possible disadvantages mentioned above. Two methods of using whole blood are, therefore, described first; the use of anticoagulants is then described in detail, and their advantages and possible dangers are enlarged upon.
Whole Blood Transfusion with Syringes.—It is obvious that, if blood can be drawn from the donor’s vein into a glass syringe and injected into the recipient so rapidly that clotting has no time to occur, then a transfusion of any quantity of blood that may be wished can be given by this simple means. The measure of the amount[113] of blood transfused is given by the number of syringes that have been filled and emptied. This method has been successfully used by several workers, and it has the advantage that no very special apparatus is necessary. It does, however, require that several syringes, and more than one assistant, should be available, since clotting will take place in the syringes, unless they be frequently washed out. There is also the possibility that clotting may take place in the needle which is introduced into the donor’s vein, since this cannot be withdrawn and replaced for each syringeful of blood that is transferred. With practice, however, and with good assistants, the process can be done quickly enough to avoid this. Wide-bore needles with short rubber connexions are introduced into the veins of donor and recipient; if, as often happens, this is difficult to do through the skin in the case of the recipient, his vein must first be exposed through an incision and a glass or metal cannula introduced into it. The operator then fills the syringes with blood in quick succession and hands them to his first assistant, who injects the blood into the recipient. Blood is prevented from escaping from the needles when the syringes are disconnected by nipping the rubber connexions with the fingers. The first assistant passes the empty syringes to the second assistant, who washes them out with normal saline, and hands them back if needed to the operator. This can be done with six 20 cc. syringes used in rotation, possibly with only four.
The most recent description of this method has been published by J. M. Graham of Edinburgh, who has introduced an improved form of needle. This consists of a double tube; the inner tube has a needle point which is used for puncturing the vein, and can be withdrawn into the blunt outer tube when the vein has been entered. Any further wounding of the vein is thus avoided. In addition, movement of the needle-cannula is prevented by a bull-dog forceps attachment, which is clipped to the skin. Graham finds it advisable to lubricate the cannulæ and[114] syringes with vaseline before being used. He also states that: “As the absence of clotting depends upon the rapidity with which the syringes are filled and emptied, a series of syringes should be used in strict rotation, and all trace of blood must be washed out with saline before the syringes are used again. One or two additional assistants are necessary for this method.” The disadvantages are evident, and it is not suitable for general use.
A modification of the method has been described by Unger, in which only one syringe is used. The barrel of this is cooled by an ether spray so that clotting is discouraged or prevented.
Whole Blood Transfusion with Kimpton’s Tube.—The principle of this method depends upon the use of paraffin wax as a coating for the vessel into which the blood is drawn, so that clotting is prevented or greatly delayed. The form of the vessel has been modified by different workers, but the essentials are the same in each. One form of the apparatus, known as the Kimpton-Brown tube, is illustrated in the accompanying diagram. It consists of a graduated glass cylinder, of about 700 cc. capacity, the lower end of which is drawn out into a cannula point at an acute angle with the body of the cylinder; the point is of a size convenient for introducing into a vein and its bore large enough to allow of a free flow of blood through it. Near the upper end is a side tube to which a rubber tube can be attached, and an opening at the top is closed by a rubber bung. An ordinary rubber double-bulb bellows is the only other apparatus that is needed.
[115]
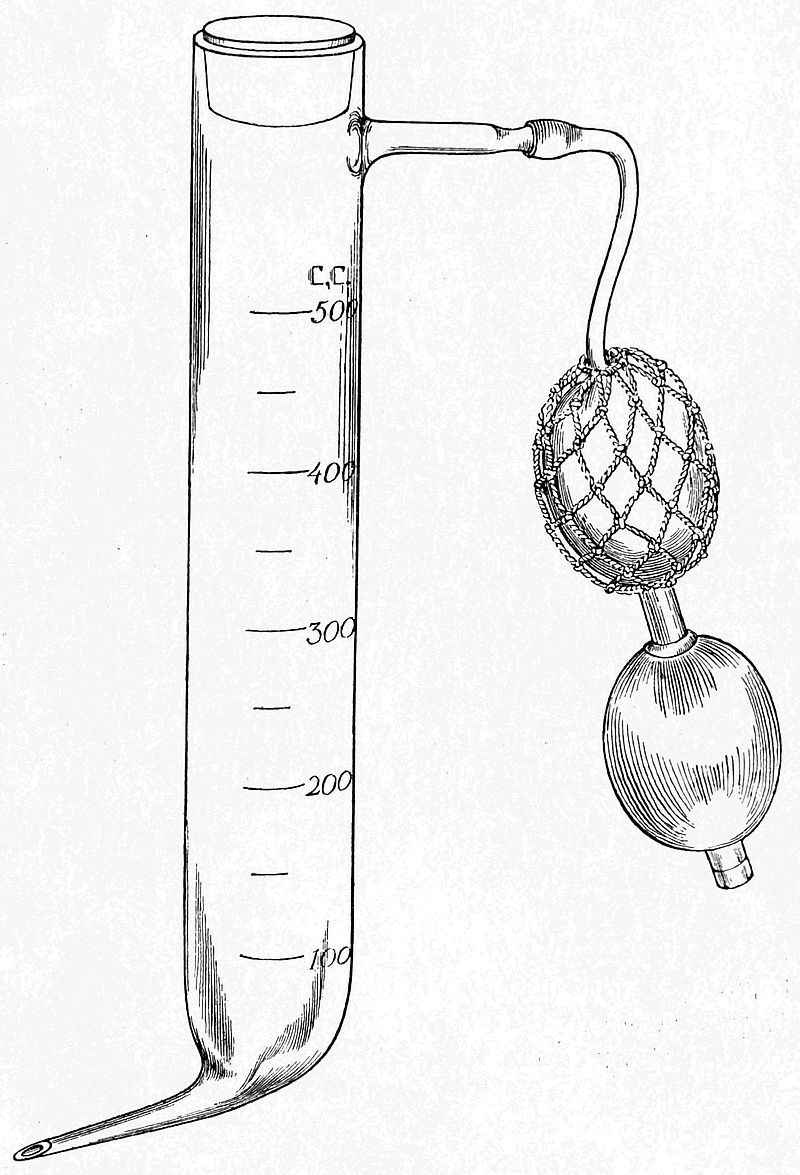
The glass vessel is first sterilized in the autoclave, and then it must be coated on the inside with a thin layer of paraffin wax. The whole success of this method depends upon this wax coating being absolutely complete right up to the tip of the cannula at the bottom. If the tiniest area of glass be left exposed in the cannula, the process will fail. The production of this perfect wax coating used to be exceedingly difficult of attainment without very frequent [116]practice. The apparatus was first raised to exactly the right temperature; sterile, melted paraffin was then put into it, and distributed evenly over the surface, excess being allowed to run out. The apparatus was then cooled down, and could be put away in a sterile towel ready for use, great care being taken that the lumen of the cannula was patent and not blocked with excess of wax. A simplification of the process was introduced by the use of a saturated solution of wax in ether. This solution is put into the vessel, which must not be heated, and is made to run all over the surface, excess as before being allowed to escape through the lower opening. The ether quickly evaporates, leaving a very thin and perfect film of wax over the surface of the glass. As before, it must be ascertained that the lumen of the cannula is patent. The apparatus is then ready for use.
The donor and recipient need not be lying close together, but they must be in the same room. A vein is exposed in the arm of each by dissection under a local anæsthetic. The operator then picks up the vein with a pair of dissecting forceps, and makes an oblique cut into the lumen as in the diagram on p. 131. A flap is thus made which is held in the dissecting forceps in the left hand or is picked up with a fine-pointed pair of artery forceps. The Kimpton’s tube is taken in the right hand, and the point of the cannula is introduced into the vein; that part of the lumen lying opposite the flap serves as a gutter which guides the cannula directly into the lumen, so that it is introduced without any fumbling or delay. The cannula is pushed on so that its widest part engages the whole circumference of the vein, forming a joint through which blood does not leak. The cannula having been pushed well up into the vein, the forceps holding the venous flap may be let go. At the same time an assistant grips the donor’s upper arm, or some form of tourniquet of the necessary degree of tightness is applied, so that the veins become congested without obliteration of the arterial pulse. Blood[117] now flows rapidly into the tube, and the venous pressure is always sufficient to overcome the counter-pressure of the increasing head of fluid in the tube. It is unnecessary, therefore, to produce any negative pressure within the tube with a reversed Higginson’s syringe or an exhaustion pump, which has been used by some workers. Blood is allowed to flow into the tube until the requisite amount has been obtained. The venous congestion is then released, and at the same time the tube and cannula, held at the lower end with the right hand in such manner that the index finger is free, is withdrawn from the vein. At the moment of withdrawal the end of the cannula is closed with the right index finger. To prevent hæmorrhage from the donor’s vein, a ligature previously put round it is tied by an assistant, or pressure on it is maintained with a sterile swab. The operator must now, without a moment’s delay, carry the tube filled with blood over to the recipient. An opening in his vein is made by an assistant in the same manner as already described, the finger is removed from the cannula, and its point is instantly introduced into the vein. It is now necessary to produce some degree of positive pressure in the tube to ensure that the blood shall at once begin to flow steadily into the vein. This is done with a rubber bellows, attached by an assistant to the upper side tube, and the level of the blood in the tube should at once begin to fall. Great care must be taken that the positive pressure is released before the tube is completely emptied of blood in order to avoid the obvious danger of the entry of air into the patient’s vein. When the tube is nearly empty it is withdrawn, the vein is ligatured, and the wounds in donor and recipient are sutured. The most convenient pattern of Kimpton-Brown tube holds only about 500 cc. of blood, so that if more is needed, the process must be repeated.
There is virtually only one cause of failure in transfusion by this method, and that is the occurrence of clotting in the cannula or at the bottom of the tube. If it does occur[118] at any stage of the operation, it cannot be remedied. It may happen when the tube is nearly full; if so, the blood that has been withdrawn cannot be used. Clotting may be due to an imperfection in the paraffin coating on the glass, but if there is any delay from any cause, it may take place independently of this. The method is therefore never absolutely certain of success even in the hands of an expert, and for general use it is certainly unsuitable. It was introduced into the British Army by some of the American surgeons in 1917, and was used by the writer under the guidance of Major Alton of the Harvard Medical Unit during the first battle of Cambrai with good results. Many of the English surgeons, however, soon abandoned it as a routine method in favour of anticoagulants. There are other objections to it besides its uncertainty. A vein must be exposed by dissection in both donor and recipient, so that avoidable injury is inflicted on the former. It is not a perfectly clean method, some blood necessarily escaping at each successive stage in the process, though an expert can reduce this to a minimum. In the hands of a novice it may occasion a very bloody scene. The whole operation is one of urgency, and the best interests of donor and recipient cannot always be considered.
Modifications have been introduced, such as that of Vincent, who uses an attachment with a needle instead of the glass cannula point. This obviates some of the objections, but introduces other difficulties, such as the necessity for coating the inside of the needle with paraffin wax. The technique can certainly be acquired, and the method has rendered excellent service in the past, but it has no obvious advantages except the uncertain one of avoiding chemical treatment of the blood.
Transfusion with Anticoagulants.—It will have become evident from the descriptions of the transfusion of whole blood already given, how great a difficulty is introduced into the technique of these methods by the physiological process of clotting in blood outside the body.[119] It is clear how much the process of transfusion would be simplified if the clotting were to be prevented. Something has already been said in the historical sketch of the various means by which this problem was attacked, and it need only be stated here that the most suitable substance for this purpose has been found to be sodium citrate. This method was introduced by Lewisohn as recently as 1915, and it soon became the method of choice among most of those who tried it.
The process of the formation of a blood clot has always been one of the great problems of physiology, and numerous theories have been propounded to explain it. The theory accepted at the present time regards the process as a complicated one depending on the presence in the blood of a number of different factors. This theoretical explanation may be represented diagrammatically as follows:
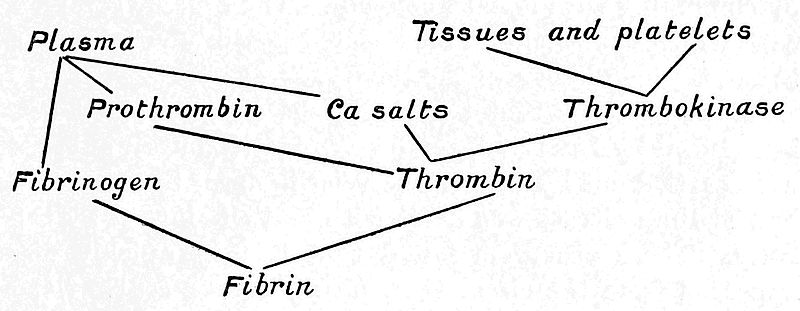
The clot consists of fibrin in which blood corpuscles are entangled. It is clear that if any one of the reacting agents can be removed or rendered inert the clotting cannot take place. There is only one inorganic substance taking part in the reaction, and it is this factor that is more easily removed than any of the others. Calcium is precipitated in an insoluble form by various chemical reagents, but it is obvious that for purposes of transfusion the formation of an insoluble precipitate is not permissible. It is therefore necessary to use a substance which will form a soluble[120] compound with the calcium and which is at the same time harmless when introduced into the circulation. The only substance which has been found at present to possess both these properties is citrate of sodium. This forms with calcium a soluble double salt, in which calcium is rendered inert. It is usually held that the calcium to be active must be present in the ionized form, but recent investigations by Vines into the rôle of calcium tend to modify slightly the accepted view of its action. He has shown that calcium is present in the blood in two forms, ionized and combined, and that both take part in the coagulation reaction. He has, in addition, demonstrated that a quantity of anticoagulant sufficient to combine with the whole of the calcium present in a given quantity of blood is not enough to prevent coagulation. It seems, therefore, that the anticoagulant acts by combining with a large organic molecule of which calcium is only one constituent, and not merely by combining with ionized calcium. The organic complex with which the calcium is associated possibly corresponds to the thrombokinase of the theory.
About the time that the use of the citrated blood was introduced by Lewisohn, some investigations upon animals were carried out by Salant and Wise in order to determine how sodium citrate was dealt with and eliminated by the body. These observers found that it very quickly disappeared from the circulation, nearly 90 per cent. of the salt having been got rid of within ten minutes of its intravenous injection. Part of the citrate is destroyed by oxidation, and the rest, 30 to 40 per cent., is eliminated by the kidneys, the urine being rendered alkaline. It was also shown that if a very large dose was given, so large that toxic symptoms resulted, the effect was rapidly obtained; but that if the toxic dose were not fatal, no remote effects followed. Its injection never resulted in any albuminuria.
Lewisohn showed by experiment on the human subject that up to 5 grammes of sodium citrate in the form of a 0·2 per cent. solution could be injected intravenously with[121]out any harmful results. It was also shown that this concentration of the salt was sufficient to prevent clotting outside the body, and that the microscopic appearance of the blood cells was not altered by the admixture of this solution.
Theoretically, therefore, the amount of citrate that should be used as an anticoagulant should be 2 grammes for 1,000 cc. of blood, or 100 cc. of 2 per cent. solution for 900 cc. of blood. In practice it is better to err on the side of safety and to use a slight excess of citrate. This amount of citrate should be used for the 750 cc. of blood which constitutes the ordinary maximum amount of blood used in a transfusion. For smaller quantities of blood the amount of citrate may be correspondingly reduced.
The use of citrated blood was introduced to the British Army in France in 1917 by Oswald Robertson, who recommended the use of a larger amount of citrate than this. His object in increasing the amount was to produce a solution which, when diluted with the correct amount of blood, would be isotonic with it. It was thought that a hypotonic solution might result in some damage to the red corpuscles by osmosis, and Robertson therefore recommended the use of 160 cc. of a 3·8 per cent. solution of citrate, which, when mixed with 750 cc. of blood, will give a solution of which the osmotic pressure equals that of 0·9 per cent. saline solution. It may be doubted, however, whether this consideration is of more than theoretical importance. There can be little doubt that in practice the effect of a slightly hypotonic solution, such as is given by the 100 cc. of 2 per cent. solution of citrate, is negligible as regards destruction of corpuscles. If, however, it be thought necessary, an isotonic solution may be produced by the addition of sodium chloride. Other considerations, as will be seen shortly, weigh in favour of giving the smaller amount of citrate. The dosage to be recommended, therefore, on practical and experimental grounds is 2 grammes of citrate in 100 cc. of water for 900 cc. of blood,[122] or 1 gramme of citrate in 50 cc. of water for 450 cc. of blood or less. These proportions need not be observed very accurately. Latitude may be used in either direction without harming either the transfused blood or the patient.
It has been stated above that sodium citrate introduced into the circulation in small quantities, such as are sufficient for anticoagulant purposes, is non-toxic to man. In the light, however, of the extended experience of the last four years, it is seen to be possible that this statement may not be quite literally true. Probably there is an individual variation in the tolerance of different people to sodium citrate. Certainly in some cases a reaction follows the injection of citrated blood. The symptoms of this reaction are a slight headache, a rise in temperature to two or three degrees above normal, sometimes accompanied by a rigor or a sensation of chill, and an increase in the pulse rate. The effect is, however, always very transitory, lasting only two or three hours, and is never, in my own experience, attended by any symptoms which need give rise to anxiety for the patient’s welfare; nor does it in any way prejudice the therapeutic results of the transfusion.
That the reaction is caused by the citrate and not by another constituent of the transfused blood has been believed by several observers. In a case seen by the writer a slight citrate reaction occurred in a youth who acted as blood donor. The transfusion was carried out by a modification of the syringe method, which involved the injection at intervals of a syringeful of citrate solution into the donor’s circulation. The possibility that the reaction was produced by another factor was therefore not present in this instance.
Nevertheless, it must be admitted that citrate has not yet been absolutely proved to be the cause of this slight reaction in all the cases in which it occurs. Evidence has, indeed, been brought forward by Lewisohn and by Meleney to show that citrate is definitely not responsible for the[123] reaction. The statement is made that some reaction occurs after 10 per cent. of all transfusions, and that this percentage is unaffected whether whole blood or citrated blood is used. Lewisohn has himself investigated the effects in a long series of parallel cases in which different methods were employed, and he reports that the results following the use of citrated blood were as good as with any other method. Drinker states that reactions follow the use of citrated blood slightly more often than they do that of whole blood, but this has not been confirmed. He was unable to find any impurity in the citrate that might be held responsible. It is quite possible that all the reactions observed are in reality caused by the “minor agglutinins” mentioned on p. 73. Meleney has noticed that the blood of some donors is more likely to produce a reaction than that of others; this suggests that the responsibility rests with the blood and not with the citrate. The occurrence of a toxic reaction constitutes the only real objection to the use of citrated blood that has yet been brought forward, but even this has not yet been fully substantiated; in any case, the reaction is of so little importance that it is greatly outweighed by the numerous advantages that are conferred by the use of citrate. The possibility that a citrate reaction does sometimes occur may be taken as an indication in favour of using the smaller amount recommended by Lewisohn rather than the larger dose used by Robertson. The experience of a great many observers has established the fact that citrated blood is quite as effective as whole blood in its therapeutic effects.
It is convenient to have the sodium citrate in a form ready for immediate use. I have therefore been in the habit of keeping it in the solid form in small stoppered bottles, each containing 1 gramme of the salt. These are sterilized at 130° C., and can be kept indefinitely until wanted. If 450 cc. of blood or less are to be drawn, the contents of one bottle is shaken into the transfusion flask; 50 cc. (approximately 2 oz.) of sterile warm water are[124] added, in which the citrate will rapidly dissolve. If more than 450 cc. of blood is to be used, the contents of two bottles must be dissolved in 100 cc. or 4 ozs. of water. Alternatively a concentrated solution of citrate may be kept in sealed ampoules, but the salt is less stable in solution, and I prefer to keep it in the solid form.
The ideal method of blood transfusion seems to me to require that it shall be absolutely certain of success, that the blood shall not necessarily be injected into the patient immediately it has been drawn, so that other circumstances besides the demands of the transfusion operation can be considered, and that no injury shall be done to the donor beyond the puncturing of a vein. In addition to this, the method should be so simple and free from special apparatus that it can be easily learnt and carried out by one operator without skilled assistance. All these requirements are fulfilled by the citrate method, and a satisfactory method of performing this will next be described. As will be seen, the blood can be drawn with the minimum amount of injury to the donor; when drawn, it can be put on one side, for several hours if necessary, and then given to the patient at whatever may be judged to be the most favourable moment; the whole process can be carried out by a single operator without any assistance; and finally, but little practice is needed to make success certain every time.
The transfusion apparatus known as “Robertson’s bottle,” first described by Oswald Robertson in 1918, is the basis of most citrate methods. This could be easily improvised in a field laboratory, and was extensively used during the last year of the war. The apparatus consisted of a glass bottle of about a litre capacity, the mouth of which was closed by a rubber bung. Through the bung three glass tubes passed. One, connected by a short rubber tube with a wide-bore needle, ended about an inch from the bottom of the bottle; through this the blood flowed into the bottle. A second tube, which reached to the angle between the side and the bottom of the bottle,[125] was connected by a rubber tube with a cannula; through this the blood was injected into the patient. The third tube reached only just beyond the bung, and to this was attached a Higginson’s syringe, by means of which either negative or positive pressure would be produced inside the bottle, according to which end of the syringe was attached.
It is unnecessary to describe this apparatus any further, for it was found by myself and others that it could be with advantage modified in the direction of simplicity. It is in the first place unnecessary in drawing the blood to create any negative pressure if a needle of a large enough bore (2 or 3 mm.) be used, and, further, it is an advantage not to have the needle attached in any way to the bottle, which, as the blood flows into it, has to be freely agitated in order to mix the blood quickly with the citrate. The needle may, therefore, be attached to a rubber tube of suitable length which hangs freely into the collecting vessel as shown in the diagram on p. 127. The third tube of “Robertson’s bottle” may be dispensed with by using a conical flask provided with a side tube to which a rubber bellows can be attached. The delivery tube is therefore the only one that need pass through the rubber bung. This tube should have an angle in it inside the flask so that its lower end reaches into the corner, and the extremity should be ground down obliquely so that, although it reaches right into the corner, it does not become occluded by too accurate contact with the surface of the vessel. By this means any wastage of blood is prevented. I have found it a very great convenience to introduce into the delivery tube just outside the flask an air-lock,[8] the value of which will be seen shortly. To the barrel of this air-lock a rubber tube with a cannula is attached. Close to the cannula is some form of clip. The whole apparatus is illustrated in the figure on p. 133, and with the help of this its use may be readily understood.
[126]
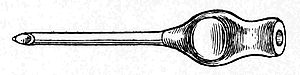
The particular form of needle which I have been in the habit of using is shown in the figure. Its lumen has a diameter of 2 mm., and the steel tube ends off flush with the wide shoulder to which the rubber tube is attached. This avoids any recess within the needle in which clotting may begin. The point of the needle should not be too long, in order that it may not wound the opposite side of the vein when it has been introduced. For ease of introduction, however, the extremity should be very sharp and should have cutting edges. The point and edges should be touched up on a bevelled hone each time before the needle is used. The needle should be kept ready for immediate use in liquid paraffin. I have found that the most convenient way of keeping it is to put it into a test-tube containing paraffin, which is plugged with cotton-wool and sterilized at 130° C. in the hot air oven or by careful heating over a flame. In this way the needle may be kept ready for an indefinite time without any chance of its rusting. When it is taken out of the test-tube, a sterile rubber tube is slipped on to it and it is then ready for use. As an additional precaution, a small quantity of paraffin may be drawn up into the rubber tube, which is thus lubricated on the inside, but this is not absolutely necessary. The tube must be sterilized with the rest of the apparatus, as rubber is destroyed by liquid paraffin.
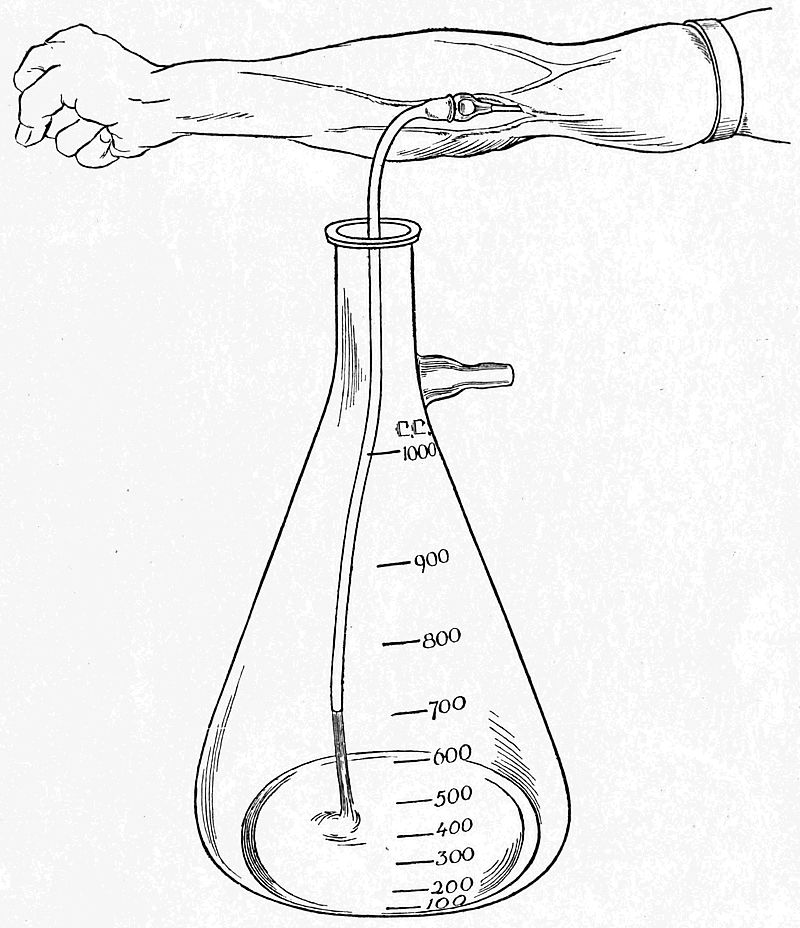
When the donor’s arm has been congested by gripping it above the elbow, or better by the application of a tourniquet[9] drawn to the requisite degree of tightness, a suitable vein, usually the median basilic, is chosen. The[127] area of puncture is washed with ether and a very small quantity, 2 to 3 minims, of 2 per cent. novocain is introduced over the vein with a hypodermic syringe. If a larger quantity is used, the vein may become obscured, but this small amount may be dispersed by a few moments’ pressure with the finger, and is usually enough to anæsthetize the very small area of skin that is to be operated upon. A tiny cut in the skin is then made with the point of a scalpel, and the needle is pushed through into the vein. If the donor’s vein is a large one, such as is usually found in the type of[128] donor recommended in a previous chapter, this is quite easy to do. To make it equally easy if the vein be smaller, it has been suggested by Watson that the vein may be fixed by pushing an ordinary fine sewing-needle through the skin at right angles to the line of the vein, into the vein, and out again through the skin. This needle is held with the forefinger and thumb of the left hand, while the right hand pushes the transfusion needle into the lumen of the vein just below it. When the needle is in the vein, the blood flows out rapidly through the tube which hangs into the flask containing the citrate, as illustrated. This flask is held by an assistant, who mixes the blood with the citrate by gently swinging it. If a properly adjusted tourniquet is kept on the donor’s arm while he works his forearm muscles by clasping and unclasping his hand, a flow of blood is obtained which is fast enough to prevent clotting in the needle, and indeed is quite as fast as most donors can tolerate. Blood up to 1,000 cc. may be collected in this way in ten to twenty minutes. If the vein be of a good size, it makes no difference whether the needle be inserted towards the heart or away from it. When enough blood has been collected, the tourniquet is removed, the needle is withdrawn, and pressure is maintained with a sterile swab over the site of puncture for a few minutes. No further bleeding will take place after this, and no suture is needed. The donor’s part in the operation is then finished. He should be made to lie on his back for a few hours afterwards, and given plenty of fluids, but beyond this no special precautions are necessary.
When the blood has been drawn, and has been satisfactorily mixed with the citrate, the flask may be put on one side until it is wanted, its mouth having been closed with a cotton-wool stopper. If the blood is wanted at once, the flask may be stood in a basin of warm water to keep it at body temperature. Otherwise it may be allowed to cool, and can be warmed up again when it is to be administered. The citrated blood may be kept for a con[129]siderable time without undergoing any appreciable change in its therapeutic value. It has been given twelve hours or more after being taken with the same good effects as if it had been newly drawn. During the war advantage was taken of this fact to anticipate during quiet times the necessity for many transfusions during times of stress. The blood was drawn in some quantity and kept for several hours in an ice chest, so that it was readily available during the expected battle. Recently I have administered to a woman who had been operated upon for a ruptured ectopic gestation 600 cc. of citrated blood which had been kept for twenty-seven hours at room temperature after it was drawn. The effect was in every way as satisfactory as if it had been freshly drawn, and there was no sign of any toxic reaction. So far as I know, blood had not ever been kept so long as this before being used, but there does not seem to be any objection to so doing.
When the blood is to be given, the delivery tube with the rubber bung is inserted in the flask, and the corpuscles which have gravitated to the bottom are distributed again through the fluid by gently shaking it. In administering the blood, it is very often advisable to inject it through a cannula which is tied into a vein. If the patient is a woman, it will usually be found that the veins are small and buried in fat. Also many transfusions will be given to combat the collapse due to shock and hæmorrhage, in which case the veins will be empty and the use of a cannula will be found essential. Sometimes, however, the patient will have large veins which can be readily distended; this may sometimes be encouraged by keeping the arm for half an hour beforehand in a bath of hot water. Under these circumstances the blood can be given through a needle introduced in exactly the same way as has already been described in the case of the donor. In the following account of the process it will be assumed that the use of a cannula is necessary.
When choosing a vein in the patient, the operator must be[130] guided by circumstances. Usually the median basilic will be the most convenient, and if, in a collapsed patient, this is invisible, previous knowledge of the position of the vein must determine the site of the incision. If another operation is being done simultaneously upon the upper part of the patient’s body, it may be more convenient to use the internal saphenous vein in Scarpa’s triangle, or even one of the superficial veins about the ankle. In administering blood to an infant, several methods have been used. These are described separately at the end of the present chapter.
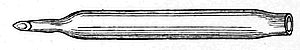
Whatever vein be chosen, the line of the incision is first infiltrated with a small quantity of a 2 per cent. solution of novocain. The vein is then dissected out, and is ligatured near the lower end of the incision. A ligature is also put loosely round the upper part. The operator now takes the barrel of the air-lock, which, together with the attached rubber tube and cannula, is filled with 0·9 per cent. saline solution, all air bubbles being carefully excluded. The tube is clipped near the cannula, so that the whole system, including the cannula, remains filled with the fluid. The form of the cannula used will depend upon the operator’s particular preference, but a type which I have found very convenient is shown in the accompanying figure. It is made of glass, and its extremity is ground down at an angle, which makes it very easy to introduce into the vein. The slight constriction near this end ensures that it can be securely tied into the vein and that no leakage round it shall occur. This is very necessary, because there is sometimes a considerable pressure to be overcome, due to venospasm in a collapsed patient, before the blood begins to flow.
An oblique cut is now made in the vein, as shown in the[131] illustration, the cannula is introduced, and the upper ligature is tied.
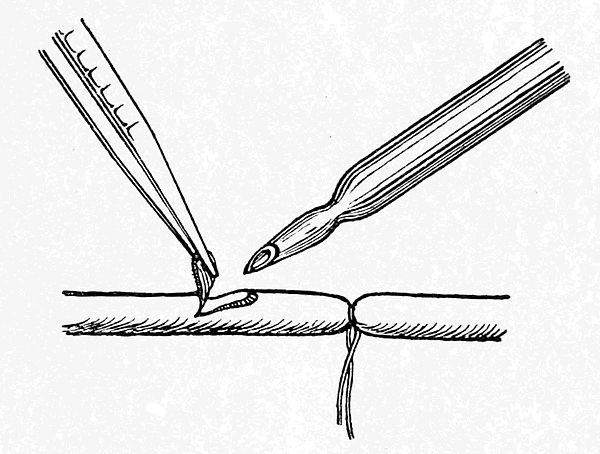
The barrel of the air-lock, with its contained saline solution, is then fixed firmly on to the rubber bung, so that the nozzle of the delivery tube projects into the saline solution. Meanwhile, an assistant has fixed a rubber bellows on to the side tube of the flask; a short piece of glass tubing loosely packed with cotton-wool should be interposed between the bellows and the flask to prevent any particles of dust being blown over into the flask from the bellows, which is not sterilized. The clip near the cannula is released, and some positive pressure is produced inside the flask by means of the bellows. The citrated blood then rises in the delivery tube, and a corresponding quantity of saline solution is displaced from the air-lock into the patient’s circulation. The blood then flows from the nozzle of the delivery tube into the air-lock, and the remainder of the saline solution is driven on into the patient. Finally the blood flows steadily through the cannula, and the rate at which it is flowing can be observed in the air-lock.
The presence of this air-lock facilitates, as has been seen, the introduction of the cannula, into the vein, since there is no leakage of blood to obscure the operation. In addition, the operator can see at a glance whether the blood is[132] flowing in properly, and can regulate the rate of flow to a nicety by varying the pressure in the flask by means of the bellows. If a very slow injection is required, the blood can even be made to run drop by drop. If the patient is suffering from acute anæmia, the blood can be pumped in rapidly, 750 cc. of blood being given in the course of twenty minutes. If, on the other hand, the patient has a plethora of fluids, such as is seen in some cases of secondary anæmia, the blood must be given very much more slowly than this, since it is dangerous rapidly to increase the blood volume. A half to three-quarters of an hour must be occupied in giving 500 cc., and even then the patient may complain of a sensation of tightness in the chest and of dyspnœa, due to embarrassment of the right heart during the transfusion. This complaint, however, is usually transient, and will disappear quickly if the injection be stopped for a few minutes.
It has been said that the lower end of the delivery tube reaches into the angle between the side and the bottom of the flask. When therefore the flask is nearly empty, it should be tilted so that very nearly the whole of the blood can be forced up the tube. When the flask is quite empty, the blood in the barrel of the air-lock must be carefully watched, and when its level has fallen to the bottom of this, the clip must be applied to the tube above the cannula. By this means no blood is wasted except the small quantity which remains in the tube below the air-lock. As soon as the tube has been clipped the cannula is withdrawn, the vein is ligatured above the opening into its lumen, and the edges of the skin incision are sutured.
Transfusions carried out in this way can be performed with uniform success. The technique is simple and straightforward at every stage, and can be easily demonstrated and learnt. It is, in addition, a perfectly clean process, and not a single drop of blood need be spilt. Any method which involves the injection of blood under pressure is open to the objection that it is possible to over[133]look the fact that the flask has been emptied and to kill the patient by injecting air into his veins. This can, however, only happen as the result of great carelessness on the part of the operator. The presence of the air-lock affords an additional safeguard, as it can hardly escape the operator’s notice that blood has ceased to flow from the nozzle of the delivery tube.
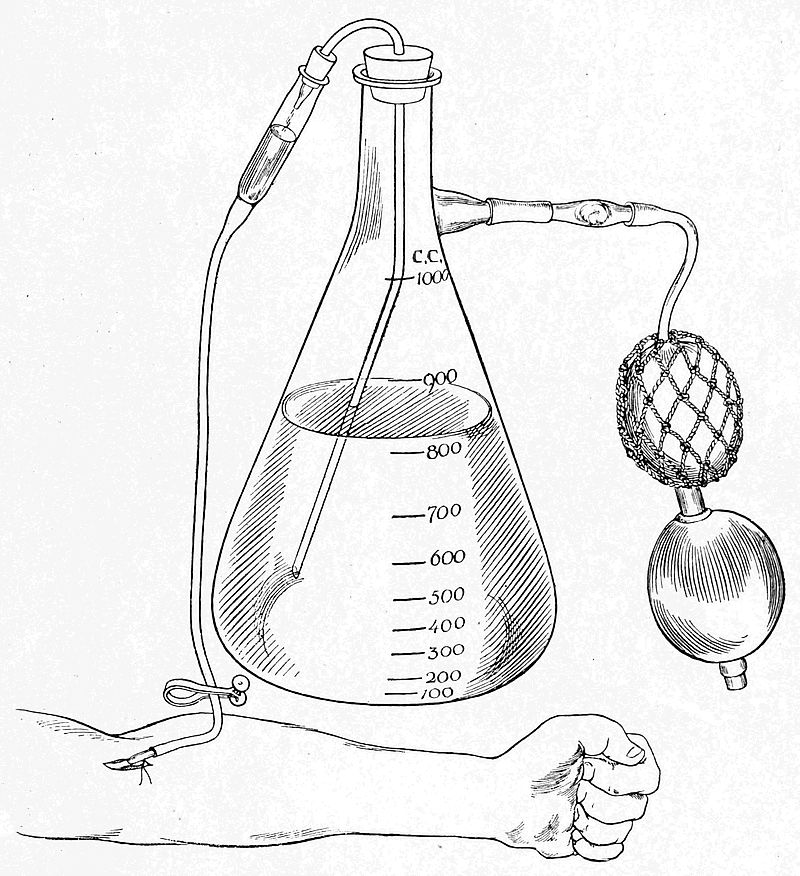
The method may also be criticized on the ground that some damage is caused to the corpuscles of the donor’s blood by the shaking which is necessary to mix it with the[134] citrate solution. This objection is, in my opinion, theoretical rather than practical. If, however, it be desired to avoid any such shaking, the apparatus designed by A. E. Stansfeld and described by him in 1918 may be used. This ensures that the citrate and the blood flow into the containing vessel together, so that no further mixing is needed. The apparatus is more cumbrous, more fragile, and less easy to clean and to sterilize than that described above. In the hands of an expert it will give excellent results, but its use requires some little practice, and it is therefore not so well adapted for general use.
The whole of my own apparatus, as described above, may be obtained from Messrs. Allen & Hanburys, Wigmore Street, London, W.1, who also provide a convenient box for carrying it.
Transfusion of Infants.—The technique of transfusions performed upon children over the age of about four years does not differ from that used for adults, except that less blood is to be given. The antecubital veins are much smaller and a finer cannula may have to be used, but this is the only source of trouble. The transfusion of infants and very young children may, however, be found to be much more difficult. The operation will have to be done for conditions such as melæna neonatorum, which was discussed on p. 48 of the present work, or for post-operative collapse, such as may follow an operation for congenital hypertrophic stenosis of the pylorus, for intussusception, or for some of the more extreme cases of harelip and cleft palate. In all such instances the transfusion will be a matter of some urgency. Speed and certainty will depend on previous knowledge of the best method to be employed.
In the case of melæna neonatorum treated by R. D. Laurie, which has been already referred to, a needle was introduced into one of the antecubital veins, and 20 cc. of citrated blood were injected with a syringe. This method,[135] however, is not to be recommended, on account of its great difficulty.
The method used by Helmholtz and also by Howard depends on the introduction of a syringe needle into the superior longitudinal sinus through the anterior fontanelle. A needle two to three inches long attached to a 20 cc. syringe is inserted near the upper angle of the fontanelle at an angle of about 25° with the scalp. As the needle pierces the wall of the sinus, a sensation of resistance is experienced, similar to that given by the piercing of the dura mater in doing a lumbar puncture. Blood should then be allowed to enter the syringe in order to demonstrate that the point of the needle really is lying in the sinus. Abnormalities have occasionally been met with, in which the sinus was situated to one side of the middle line or was very much smaller than usual. The danger of injecting the blood in such a case into the brain or the subdural space need not be emphasized. Difficulty may also be caused by restlessness on the part of the child, and to overcome this Helmholtz has devised an apparatus which grips and fixes the child’s head at a suitable angle. All this, however, makes the process unnecessarily elaborate. As an alternative, Vincent has exposed one of the internal jugular veins into which he introduces a cannula. This again is a comparatively difficult operation, which may leave a permanent scar in a conspicuous place. Vincent had previously used the femoral vein, but he found this difficult to approach, and the wound was apt to become contaminated afterwards.
The method of choice is undoubtedly that used by Bruce Robertson, who has performed a much larger number of transfusions upon infants and children than any other worker in this field of surgery. He has found that the internal saphenous vein near the ankle is a vessel possessing a fairly wide lumen and thick walls even in infants, so that a needle or cannula can be introduced into it with comparative ease and rapidity. The vein must, of course,[136] be freely exposed through an incision, but its situation removes any objection there might otherwise be to this operation. Robertson has usually employed the syringe-cannula method described earlier in the present chapter, but there is no objection to the use of an anticoagulant. The small amount of blood to be given, 15 cc. per pound of body weight, makes the use of the transfusion flask unnecessary. It is better to use a 20 cc. syringe, into which 2 cc. of a 10 per cent. solution of sodium citrate is drawn as a preliminary. The needle in the donor’s vein and the cannula in the infant’s saphena should each be provided with a rubber connexion, which can be clipped, or pinched by an assistant, when the syringe is not attached. The syringe containing the citrate is filled with blood and injected into the infant as often as may be necessary until the total amount decided upon has been given.
Robertson has used this method for complete replacement of the circulating blood in treating streptococcal septicæmia following erysipelas, and for shock in children due to burns. The infant’s blood is removed through the anterior fontanelle, while a fresh supply is injected into the saphenous vein. Complete replacement has not, so far as I know, ever been performed upon an adult, but the process is feasible, given a large enough assemblage of donors. In this way some vieillard might attempt the rejuvenation, which at present, as we are told, has only been obtained from the transplantation of “monkey glands” by Viennese professors.
[137]
1. ADDIS, T.: “The effect of intravenous injections of fresh human serum and of phosphated blood on the coagulation time of the blood in hereditary hæmophilia.” Proc. Soc. Exp. Biol. and Med., 1916, xiv. 19.
2. AGOTE, L.: “Nuevo procedimiento para la transfusión del sangre.” Anales del Inst. modelo de clin. med. Buenos Ayres, Jan. 1915.
3. ALBINI: “Relazione sulla trasfusione diretta di sangue d’agnello.” Naples, 1873.
4. ALEXANDER, W.: “An enquiry into the distribution of the blood groups in patients suffering from malignant disease.” Brit. Journ. Exp. Path., 1921, ii. 66.
5. ANDERS, J. M.: “Transfusion of blood in pernicious anæmia.” Am. Journ. Med. Sci., 1919, clviii. 659.
6. ARCHIBALD, A.: “The transfusion of blood in the treatment of pernicious anæmia.” St. Paul Med. Journ., 1917, xix. 43.
7. ASHBY, W.: “The determination of the length of life of transfused blood corpuscles in man.” Journ. Exp. Med., 1919, xxix. 267. (Also in Collected Papers of the Mayo Clinic, xi., 1919.)
8. AVELING, J. H.: “An improved apparatus for immediate transfusion.” Med. Rec., 1874, ix. 190.
9. BARRIS, J., & DONALDSON, M.: “Acute inversion of the uterus. Treatment by blood transfusion and late replacement.” Proc. Roy. Soc. Med., Obstet. Sect., 1921, xiv. 207.
10. BAYLISS, W. M.: “Intravenous injection in wound shock.” Longmans, Green & Co., 1918.
11. BAYLISS, W. M.: “Intravenous injections to replace blood.” Rep. of the Med. Res. Com., i., 1919, 11.
12. BAYLISS, W. M.: “The toxicity of hæmolysed blood.” Brit. Journ. Exp. Path., 1920, i. 1.
[138]
13. BAYLISS, W. M., and others: “Acidosis and shock.” Rep. of the Med. Res. Com., vii., 1919, 245.
14. BAZETT, M. C.: “The value of hæmoglobin and blood pressure observations in surgical cases.” Rep. of the Med. Res. Com., v., 1919, 181.
15. BELINA, DE: “De la transfusion du sang défibriné.” Paris, 1873.
16. BELKNAP, R. W.: “Suggestions for identification of blood groups.” Journ. Am. Med. Assoc., 1921, lxxvi. 724.
17. BELL, W. B.: “The treatment of eclampsia by transfusion of blood.” Brit. Med. Journ., 1920, i. 625.
18. BENEDICT, N. B.: “On the operation of transfusion—being the report of a committee.” New Orleans Med. and Surg. Journ., 1853, July.
19. BERARD, L., & LUMIÈRE, A.: “Technique for transfusion of blood.” Presse Méd., 1915, xxiii. No. 41.
20. BERNHEIM, B. M.: “An emergency cannula.” Journ. Am. Med. Assoc., 1912, lviii. 1007.
21. BERNHEIM, B. M.: “Therapeutic possibilities of transfusion.” Journ. Am. Med. Assoc., 1913, lxi. 268.
22. BERNHEIM, B. M.: “Hæmolysis following transfusion of blood; a study.” Lancet-Clinic, 1915, cxiii. 259.
23. BERNHEIM, B. M.: “A simple instrument for the indirect transfusion of blood.” Journ. Am. Med. Assoc., 1915, lxv. 1278.
24. BERNHEIM, B. M.: “The limits of bleeding considered from the clinical standpoint.” Am. Journ. Med. Sci., 1917, cliii. 575.
25. BERNHEIM, B. M.: “Blood transfusion, hæmorrhage and the anæmias.” Lippincott Co., 1917.
26. BERNHEIM, B. M.: “Whole blood transfusion and citrated blood transfusion. Possible differentiation of cases.” Journ. Am. Med. Assoc., 1921, lxxvii. 275.
27. BISCHOFF, T. L. W.: “Beiträge zur Lehre von dem Blute und der Transfusion desselben.” Arch. f. Anat. Physiol. u. wissensch. Med., 1835, 347.
28. BLASIUS: “Statistik der Transfusion des Blutes.” Monatsbl. f. med. Statist. u. öff. Gsndhtspleg. Berlin, 1863, 77.
[139]
29. BLOOMFIELD, A.: “The results of treatment in pernicious anæmia.” Johns Hopkins Hosp. Bull., 1918, xxix. 101.
39. BLUNDELL, J.: “Experiments on the transfusion of blood by the syringe.” Med. Chirurg. Trans., 1818, ix. 56.
31. BLUNDELL, J.: “Some account of a case of obstinate vomiting, in which an attempt was made to prolong life by the injection of blood into the veins.” Med. Chirurg. Trans., 1819, x. 296.
32. BLUNDELL, J.: “Some remarks on the operation of transfusion.” Researches Physiological and Pathological. London, 1824.
33. BOND, C. J.: “On auto-hæmagglutination.” Brit. Med. Journ., 1920, ii. 925, 973.
34. BOWCOCK, H. M.: “Serious reactions to repeated transfusions in pernicious anæmia.” Johns Hopkins Hosp. Bull., 1921, xxxii. 83.
35. BREM, W. V.: “Blood transfusion with special reference to group tests.” Journ. Am. Med. Assoc., 1916, lxvii. 190.
36. BREWER, G. E., & LEGGETT, N. B.: “Direct blood transfusion by means of paraffin-coated glass tubes.” Surg. Gynec. and Obstet., 1909, ix. 293.
37. BRINTON, J. H.: “The transfusion of blood and the intravenous injection of milk.” Med. Rec., 1878, xiv. 344.
38. BUCHSER, J.: “A successful case of transfusion.” Med. Rec., 1869-70, iv. 337.
39. BUERGER, L.: “A modified Crile transfusion cannula.” Journ. Am. Med. Assoc., 1908, li. 1233.
40. BULGER, H. A.: “Blood changes in a case of hæmophilia after transfusion.” Journ. Lab. and Clin. Med., 1920, vi. 102.
41. BULLIARD, H.: “Modifications sanguines après transfusions.” Journ. de Physiol. et de Path. Gén., 1921, xix. 80.
42. BURMEISTER, W. H.: “Resuscitation by means of preserved living erythrocytes in experimental illuminating gas asphyxia.” Journ. Am. Med. Assoc., 1916, lxvi. 164.
[140]
43. CANNON, W. B.: “Shock and its control.” Am. Journ. Physiol., 1918, xlv. 544.
44. CANNON, W. B.: “Acidosis in cases of shock, hæmorrhage, and gas infection.” Report of the Med. Res. Com., ii. (3), 1919, 85.
45. CANNON, W. B.: “A consideration of the nature of wound shock.” Report of the Med. Res. Com., ii. (5), 1919, 109.
46. CANNON, W. B., FRASER, J., & COWELL, E. M.: “The preventive treatment of wound shock.” Report of the Med. Res. Com., ii. (6), 1919, 125.
47. CANNON, W. B., FRASER, J., & HOOPER, A. N.: “Some alterations in the distribution and character of the blood.” Report of the Med. Res. Com., ii. (2), 1919, 72.
48. CARTER, W. S.: “An experimental study of the use of sodium citrate in the transfusion of blood by direct and indirect methods.” South. Med. Journ., 1916, ix. 427.
49. CHARLES, R., & SLADDEN, A. F.: “Resuscitation work at a casualty clearing station.” Brit. Med. Journ., 1919, i. 402.
50. CHAVASSE, F. B.: “The blood group in mother and child.” Brit. Med. Journ., 1921, i. 641.
51. CHERRY, T. H., & LANGROCK, E. G.: “The relation of hæmolysis in the transfusion of babies with the mothers as donors.” Journ. Am. Med. Assoc., 1916, lxvi. 626.
52. CLOUGH, P. W. & M. C.: “Study of reactions following transfusion of blood.” South. Med. Journ., 1921, xiv. 104.
53. COLE, H. P.: “Transfusion and pellagra.” Journ. Am. Med. Assoc., 1911, lvi. 584.
54. COOLEY, T. B., & VAUGHAN, J. W.: “A simple method of blood transfusion.” Journ. Am. Med. Assoc., 1913, 435.
55. COWELL, E. M.: “The initiation of wound shock.” Report of the Med. Res. Com., ii. (4), 1919, 99.
56. COX, R.: “Blood transfusion in the seventeenth century.” Journ. Am. Med. Assoc., 1914, lxii. 222.
[141]
57. COX, T.: “An account of another experiment of transfusion, viz. of bleeding a mangy into a sound dog.” Philosophical Trans., 1667, ii. 451.
58. CRILE, G. W.: “The technique of direct transfusion of blood.” Ann. Surg., 1907, xlvi. 329.
59. CRILE, G. W.: “Hæmorrhage and transfusion.” Appleton & Co., N.Y., 1909.
60. CROTTI, A.: “Indirect transfusion of blood.” Surg. Gynec. and Obstet., 1914, xviii. 236.
61. CULPEPPER, W. L.: “Report on five thousand bloods typed, using Moss’s grouping.” Journ. Lab. and Clin. Med., 1921, vi. 276.
62. CURCHOD, H.: “Transfusion of blood.” Rev. méd. de la Suisse. Rome, 1920, xl. 666.
63. CURTIS, A. H., & DAVID, V. C.: “Transfusion of blood by a new method, allowing accurate measurement.” Journ. Am. Med. Assoc., 1911, lvi. 35.
64. DALE, H. H., and others: “Surgical shock and some allied conditions.” Brit. Med. Journ., 1917, i. 381.
65. DALE, H. H., and others: “Traumatic toxæmia as a factor in shock.” Rep. of the Med. Res. Com., viii., March 1919.
66. DARWIN, ERASMUS: “Zoonomia; or the Laws of Life.” London, 1794. 2 vols., 4o. Vol. i. p. 373; vol. ii. pp. 120, 605, 676.
67. DAVID, V. C., & CURTIS, A. H.: “Experiments in the treatment of acute anæmia by blood transfusion and by intravenous saline infusion.” Surg. Gyn. and Obstet., 1912, xv. 476.
68. DAVID, V. C., & CURTIS, A. H.: “Recent experiences with blood transfusion.” Journ. Am. Med. Assoc., 1914, lxii. 775.
69. DAWSON, P. M.: “The changes in the heart rate and blood pressures resulting from severe hæmorrhage and subsequent infusion of sodium bicarbonate.” Journ. Exp. Med., 1905, vii. 1.
70. DENYS, J.: “A letter concerning a new way of curing sundry diseases by transfusion of blood.” Philosophical Trans., 1667, ii. 489.
71. DENYS, J.: “An extract of a letter touching a late[142] cure of an inveterate phrensy by the transfusion of blood.” Philosophical Trans., 1667, ii. 617.
72. DIEFFENBACH, J. F.: “Die Transfusion des Blutes und die Infusion der Arzneien in Blutgefässe.” Berlin, 1828.
73. DIJK, H. VAN: “Malaria induced by convalescent’s serum.” Nederl. Tijdschr. v. Geneesk., 1920, ii. 1181.
74. DORRANCE, G. M.: “Indications for blood transfusion.” Am. Journ. Med. Sci., 1917, cliv. 216.
75. DORRANCE, G. M., & GINSBURG, N.: “Transfusion: history, development, present status and technique of operation.” N.Y. Med. Journ., 1908, lxxxvii. 941.
76. DRINKER, C. R., & BRITTINGHAM, H. H.: “The cause of the reactions following transfusion of citrated blood.” Arch. Int. Med., 1919, xxiii. 133.
77. DRUMMOND, H., & TAYLOR, E. S.: “The use of intravenous injections of gum acacia in surgical shock.” Rep. of the Med. Res. Com., iii., 1919, 135. “Observations on the blood pressure in gas gangrene infection.” Ibid., v. 1919, 199.
78. DUKE, W. W.: “Variation in the platelet count.” Journ. Am. Med. Assoc., 1915, lxv. 1600.
79. DUNGERN, E. VON, & HIRSCHFELD, L.: “Ueber Nachweis und Vererbung biochemischer strukturen.” Zeitschr. f. Immunitätsfschng., 1910, iv. 531; 1911, viii. 526.
80. DUNGERN, E. VON, & HIRSCHFELD, L.: “Ueber Vererbung gruppenspezifischer strukturen des Blutes.” Ibid., 1910, vi. 284.
81. DUNGERN, E. VON, & HIRSCHFELD, L.: “Ueber die Giftigkeit des Blutes nach der Injektion protoplasmatischen Substanzen und während der Schwangerschaft, und über passive Allergie gegenüber Hodensubstanzen.” Ibid., 1911, viii. 332.
82. EBERLE, D.: “Transfusion and reinfusion of blood.” Schweiz. med. Wchnschr., 1920, l. 961.
83. ELSBERG, C. A.: “A simple cannula for the direct transfusion of blood.” Journ. Am. Med. Assoc., 1909, lii. 887.
84. ELY, A. H., & LINDEMAN, E.: “Acidosis complicating[143] pregnancy. Report of a case cured by transfusion.” Am. Journ. Obstet. and Dis. Wom. and Child., July, 1916, lxxiv. 42.
85. EMSHEIMER, H. W.: “Intramuscular injections of whole blood in the treatment of purpura hæmorrhagica.” Journ. Am. Med. Assoc., 1916, lxvi. 20.
86. EPSTEIN, A. A., & OTTENBERG, R.: “A method for agglutination tests.” Arch. Int. Med., 1909, iii. 286.
87. ERLANGER, J., & GASSER, H. S.: “Hypertonic gum acacia and glucose in the treatment of secondary traumatic shock.” Ann. Surg., 1919, lxix. 389.
88. FLEMING, A., & PORTEOUS, A. B.: “Blood transfusion by the citrate method.” Lancet, 1919, i. 973.
89. FLÖRCKEN, H.: “Zur Frage der direkten Bluttransfusion durch Gefässnaht.” Zentrbl. f. Chir. Leipzic, 1911, xxxviii. 305.
90. FOLLI, FRANCESCO: “Stadera medica, nella quale oltre la medicina infusoria, ed altre novita, si bilanciano le ragioni favore voli e le contrarie alla trasfusione del sangue.” Florence, 1680.
91. FORSIUS, R.: “Severe hæmophilic intestinal hæmorrhage treated with transfusion of blood.” Finska Läkaresällskapets Handl., 1915, lvii. No. 3.
92. FRANK, R. T., & BAEHR, G.: “A new method for the transfusion of blood. An experimental study.” Journ. Am. Med. Assoc., 1909, lii. 1746.
93. FRASER, J., & COWELL, E. M.: “A clinical study of the blood pressure in wound conditions.” Report of the Med. Res. Com., ii. (1), 1919, 49.
94. FREILICH, E. B., and others: “Blood transfusion in treatment of pulmonary tuberculosis.” Illin. Med. Journ., 1921, xxxix. 32.
95. FREUND, H. A.: “A method for the transfusion of fresh normal blood.” Journ. Michigan Med. Soc., 1913, xii. 459.
96. FRY, H. J. B.: “The use of immunized blood donors in the treatment of pyogenic infections by whole blood transfusions.” Brit. Med. Journ., 1920, i. 290.
97. FRYER, B. E.: “A few remarks on the transfusion of blood, with a modification of the apparatus of Aveling.” Med. Rec., 1874, ix. 201.
[144]
98. FULLERTON, A., DREYER, G., & BAZETT, H. C.: “Direct transfusion of blood, with a description of a simple method.” Lancet, 1917, i. 715.
99. GARBAT, A. L.: “Intravenous injections of sodium citrate.” Journ. Am. Med. Assoc., 1916, lxvi. 1543.
100. GESELLIUS, F.: “Die Transfusion des Blutes.” St. Petersburg, 1873.
101. GESELLIUS, F.: “Zur Thierblut-Transfusion beim Menschen.” St. Petersburg, 1874.
102. GETTLER, A. O., & LINDEMAN, E.: “A new method of acidosis therapy. Blood transfusion from an alkalinized donor, with report of case.” Journ. Am. Med. Assoc., 1917, lxviii. 594.
103. GIFFIN, H. Z.: “A report on the treatment of pernicious anæmia by transfusion and splenectomy.” Journ. Am. Med. Assoc., 1917, lxviii. 429.
104. GRAHAM, J. M.: “Observations on the technique of blood transfusion.” Edin. Med. Journ., 1919, xxiii. 358.
105. GRAHAM, J. M.: “Transfusion of blood in cases of hæmorrhage.” Edinb. Med. Journ., 1920, xxiv. 142.
106. GRAHAM, J. M.: “Transfusion of blood in pernicious anæmia.” Edinb. Med. Journ., 1920, xxiv. 282.
107. GRUTZ, O.: “Bluttransfusion bei Morbus maculosus Werlhofi.” Berl. Klin. Wchnschr., 1921, lviii. 53.
108. GUIOU, N. M.: “Blood transfusion in a field ambulance.” Brit. Med. Journ., 1918, i. 695.
109. GURYE, G. DE: “An account of more tryals of transfusion, accompanied with some considerations thereon, chiefly in reference to its cautious practice on Man; together with a farther vindication of this invention from usurpers.” Philosophical Trans., 1667, ii. 517.
110. HAHN, M.: “Hæmophilia treated by transfusion.” Med. Rec., 1910, lxxviii. 624.
111. HALSTED, W. S.: “Refusion in the treatment of carbonic oxide poisoning.” Ann. of Anat. and Surg., 1884, Jan.
112. HAPP, W. M.: “Appearance of iso-agglutinins in infants and children.” Journ. Exp. Med., 1920, xxxi. 313.
113. HARDING, M. E.: “The toxæmic stage of diphtheria.” Lancet, 1921, i. 737.
[145]
114. HARRIS, D. T.: “The value of the vital-red method as a clinical means for the estimation of the volume of the blood.” Brit. Journ. Exp. Path., 1920, i. 142.
115. HARTWELL, J. A.: “A simple method of blood transfusion with cannula.” Journ. Am. Med. Ass., 1909, lii. 297.
116. HARTWELL, J. A.: “A consideration of the various methods of blood transfusion and its value.” N.Y. State Journ. Med., 1914, xiv. 535.
117. HASSE, O.: “Report on twelve cases of the direct transfusion of lamb’s blood.” Allgem. Wiener Medizin. Zeit., Dec. 1873. (Abstracted in the Lond. Med. Rec., Dec. 31, 1873.)
118. HÉDON, E.: “Note complémentaire sur la transfusion du sang citraté.” Presse méd., 1918, xxvi. 57.
119. HEKTOEN, L.: “Iso-agglutination of human corpuscles.” Journ. Infect. Dis., 1907, iv. 297.
120. HELMHOLZ, H. F.: “The longitudinal sinus as the place of preference in infancy for intravenous aspirations and injections, including transfusion.” Am. Journ. Dis. of Children, 1915, x. 194.
121. HICKS, J. BRAXTON: “Cases of transfusion, with some remarks on a new method of performing the operation.” Guy’s Hosp. Rep., 1869, 3rd s., xiv. 1.
122. HIGGINSON, A.: “Report of seven cases of transfusion of blood, with a description of the instrument invented by the author.” Liverpool Med. Chir. Journ., 1857, i. 102.
123. HINDSE-NIELSEN: “Nitro-benzol poisoning treated with blood transfusion.” Ugeskift f. Laeger, 1920, Sept. 9.
124. HIRSCHFELD, L., & HIRSCHFELD, H.: “Serological differences between the blood of different races.” Lancet, 1919, ii. 675.
125. HOFFMAN, M. H., & HABEIN, H. C.: “Transfusion of citrated blood.” Journ. Am. Med. Assoc., 1921, lxxvi. 358.
126. HOOKER, R. S.: “The treatment of staphylococcus septicæmia by transfusion of immune blood.” Ann. Surg., 1917, lxvi. 513.
[146]
127. HOWARD, W. S.: “A simple method of transfusion in hæmorrhage of the new-born, with report of a case.” Journ. Am. Med. Assoc., 1915, lxv. 1365.
128. HUCK, F. G.: “Changes in the blood immediately following transfusion.” Johns Hopkins Hosp. Bull., 1919, xxx. 63.
129. HULL, A. J.: “Direct transfusion of blood.” Brit. Med. Journ., 1917, ii. 683.
130. HUNT, E. L., & INGLEBY, H.: “A case of peptic ulcer with grave anæmia treated by intravenous injection of whole blood.” Lancet, 1919, i. 975.
131. HUNT, V. C.: “Reaction following blood transfusion by the sodium citrate method.” Texas State Journ. Med., 1918, xiv. 192. (Also in Collected Papers of the Mayo Clinic, x. 1918.)
132. HUSTIN: “Principe d’une nouvelle méthode de transfusion muqueuse.” Journ. méd. de Brux., 1914, xii. 436.
133. HUTCHISON, R.: “Three cases of melæna neonatorum successfully treated by the injection of whole blood.” Brit. Med. Journ., 1917, ii. 617.
134. HÜTER, C.: “Ein Fall von Kohlenoxydvergiftung; Heilung durch Transfusion.” Berl. Klin. Wchnschr., 1870, vii. 341.
135. INGEBRIGTSEN, R.: “The influence of iso-agglutinins on the final results of homoplastic transplantation of arteries.” Journ. Exp. Med., 1912, xvi. 169.
136. JANEWAY, H. H.: “An improved device for transfusion.” Ann. Surg., 1911, lxiii. 720.
137. JANSKY, J.: “Hæmatologische Studien bei psykotiken.” Klincky Sborink, 1907, viii. 85.
138. JANSKY, J.: “Recommendation by a committee that the Jansky classification of blood groups be used in preference to that of Moss on grounds, of priority.” Journ. Am. Med. Assoc., 1921, lxxvi. 130.
139. KAHN, A.: “Continuous transfusion. The production of immunity.” N.Y. Med. Rec., 1916, lxxxix. 553.
140. KARSNER, H. T.: “Laboratory problems of blood transfusion.” Journ. Am. Med. Assoc., 1921, lxxvi. 88.
141. KEATOR, H. M.: “Transfusion in case of toxæmia of early pregnancy with unusual hæmorrhagic manifesta[147]tions.” Am. Journ. Obstet. and Dis. Wom. and Child, 1912, lxv. 1003.
142. KEITH, N. M.: “Blood volume changes in wound shock and primary hæmorrhage.” Rep. of the Med. Res. Com., ix., March, 1919.
143. KEITH, N. M., ROWNTREE, L. G., & GERAGHTY, J. T.: “A method for the determination of plasma and blood volume.” Arch. Int. Med., 1915, xvi. 547.
144. KEYNES, G. L.: “Blood transfusion: its theory and practice.” Lancet, 1920, i. 1216.
145. KIMPTON, A. R., & BROWN, J. H.: “A new and simple method of transfusion.” Journ. Am. Med. Assoc., 1913, lxi. 117.
146. KIMPTON, A. R.: “Further notes on transfusion by means of glass cylinders.” Journ. Am. Med. Assoc., 1913, lxi. 1628.
147. KIMPTON, A. R.: “Transfusion. Experiences in over two hundred cases.” Boston Med. and Surg. Journ., 1918, clxxviii. 351.
148. KIMPTON, A. R., & BROWN, J. H.: “Technique of transfusion by means of glass tubes.” Bost. Med. and Surg. Journ., 1915, clxxiii. 425.
149. KING, E.: “An account of an easier and safer way of transfusing blood out of one animal into another, viz., by the veins, without opening an artery of either.” Philosophical Trans., 1667, ii. 449.
150. KING, E.: “The method of transfusing into the veines of men.” Philosophical Trans., 1667, ii. 522.
151. KING, E.: “An account of the experiment of transfusion, practised upon a man in London.” Philosophical Trans., 1667, ii. 557.
152. KING, H. H.: “Direct vein to vein transfusion.” Brit. Med. Journ., 1918, i. 498.
153. KUSH, M.: “An automatic transfusion apparatus.” Journ. Am. Med. Assoc., 1915, lxv. 1180.
154. LAMBERT, S. W.: “Melæna neonatorum, with report of a case cured by transfusion.” N.Y. Med. Rec., 1908, lxxiii. 885.
155. LANDOIS, L.: “Die Transfusion des Blutes.” Berlin, 1866. Leipzig, 1875.
[148]
156. LANDSTEINER, K.: “Ueber Agglutinationserscheinungen normalen menschlichen Blutes.” Wien. Klin. Wchnschr., 1901, xiv. 1132.
157. LAPAGE, C. P.: “Two cases of melæna neonatorum treated by injection of fresh citrated blood.” Proc. Roy. Soc. Med., 1920, xiii. Sect. Child. Dis., 158-160.
158. LAURIE, R. D.: “Melæna neonatorum treated by blood transfusion.” Brit. Med. Journ., 1921, i. 527.
159. LEARMONTH, J. R.: “The inheritance of specific iso-agglutinins in human blood.” Journ. Genetics, 1920, x. 141.
160. LEE, R. I.: “A simple and rapid method for the selection of suitable donors for transfusion by the determination of blood groups.” Brit. Med. Journ., 1917, ii. 684.
161. LEISRINK, H.: “Ueber die Transfusion des Blutes.” Samm. Klin. Vortr., No. 41. Leipzig, 1872, 235.
162. LESPINASSE, V. D.: “The treatment of hæmorrhagic disease of the new-born by direct transfusion of blood, with a clinical report of fourteen personal cases.” Journ. Am. Med. Assoc., 1914, lxii. 1866.
163. LESPINASSE, V. D.: “Technique of direct transfusion of blood, using iridio-platinum tubes.” Chicago Med. Rec., 1915, xxxvii. 589.
164. LESSER, L.: “Transfusion and autotransfusion.” Samml. Klin. Vortr., No. 86, Leipzig, 1875. Inn. Med., No. 29, p. 665.
165. LEVIN, I.: “Plastic surgery of blood vessels and direct transfusion of blood.” Ann. of Surg., N.Y., 1913, May.
166. LEWISOHN, R.: “A new and greatly simplified method of blood transfusion.” N.Y. Med. Rec., 1915, lxxxvii. 141.
167. LEWISOHN, R.: “Blood transfusion by the citrate method.” Surg. Gynec. and Obstet., 1915, xxi. 37.
168. LEWISOHN, R.: “The citrate method of blood transfusion in children.” Am. Journ. Med. Sci., 1915, cl. 886.
169. LEWISOHN, R.: “The importance of the proper dosage of sodium citrate in blood transfusion.” Ann. of Surg., 1916, lxiv. 618.
170. LEWISOHN, R.: “Modern methods of blood transfusion.” Journ. Am. Med. Assoc., 1917, lxviii. 826.
[149]
171. LEYTON, O.: “Transfusion in diseases of the blood.” Brit. Med. Journ., 1919, i. 279.
172. LIBAVIUS, A.: “Denfensio syntagmatis arcanorum chymicorum.” Frankfort, 1615, ch. iv., p. 8.
173. LIBMAN, E., & OTTENBERG, R.: “A practical method for determining the amount of blood passing over during direct transfusion.” Journ. Am. Med. Assoc., 1914, lxii. 764.
174. LIBMAN, E., & OTTENBERG, R.: “Recent observations on blood transfusion.” Tr. Coll. Phys. Phila., 1917, xxxix. 266.
175. LICHTENSTEIN: “Eigenbluttransfusion bei Extrauteringravidität und Uterusruptur.” Münch. Med. Wchnschr., 1915, lxii. 1597.
176. LINDEMAN, E.: “Simple syringe transfusion with special cannulas.” Am. Journ. Dis. of Children, 1913, vi. 28.
177. LINDEMAN, E.: “Blood transfusion. Report of one hundred and thirty-five transfusions by the syringe-cannula system.” Journ. Am. Med. Assoc., 1914, lxii. 993.
178. LINDEMAN, E.: “Reactions following blood transfusion by the syringe cannula system.” Journ. Am. Med. Assoc., 1916, lxvi. 624.
179. LINDEMAN, E.: “The total blood volume in pernicious anæmia.” Journ. Am. Med. Assoc., 1918, lxx. 1292.
180. LITTLE, G. F.: “Transfusion of antibacterial blood. Report of case.” Journ. Am. Med. Assoc., 1920, lxxiv. 734.
181. LOSEE, J. R.: “Blood transfusion.” Am. Journ. Med. Sci., 1919, clviii. 711.
182. LOSEE, J. R.: “Blood transfusion in obstetrics.” Med. Rec., 1920, xcvii. 265.
183. LÖWENTHAL, W.: “Ein Beitrag zur Lehre von der Transfusion des Blutes.” Berl. Klin. Wchnschr., 1871, viii. 487.
184. LOWER, R.: “The method observed in transfusing the blood out of one animal into another.” Philosophical Trans., 1666, i. 353.
[150]
185. McCLURE, R. D.: “Pernicious anæmia treated by splenectomy, and systematic, often-repeated transfusion of blood. Transfusion in benzol poisoning.” Journ. Am. Med. Assoc., 1916, lxvii. 793.
186. McCLURE, R. D., & DUNN, G. R.: “Transfusion of blood. History, methods, dangers, preliminary tests, present status. Report of one hundred and fifty transfusions.” Johns Hopkins Hosp. Bull., 1917, xxviii. 99.
187. McGRATH, B. F.: “A simple instrument for [direct] transfusion.” Journ. Am. Med. Assoc., 1914, lxii. 40.
188. McGRATH, B. F.: “Vascular suture in transfusion.” Journ. Am. Med. Assoc., 1914, lxii. 1326.
189. McGRATH, B. F.: “A simple apparatus for transfusion by the aspiration-injection method.” Surg. Gynec. and Obstet., 1914, xviii. 376.
190. MADGE, H. M.: “On transfusion of blood.” Brit. Med. Journ., 1874, i. 42.
191. MANN, F. C.: “Experimental surgical shock. The treatment of the condition of low blood pressure, which follows exposure of the abdominal viscera.” Am. Journ. Physiol., 1919, l. 86. (Also in Collected Papers of the Mayo Clinic, 1919, xi. 1225.)
192. MARTIN: “Ueber eine mit günstigem Erfolge bei einer lebensgefährlichem Intrauterinblutung vollzogene Transfusion.” Monatschr. f. Geburtsk. u. Frauenk., 1861, xvii. 269.
193. MARTIN: “Iso-agglutination beim Menschen.” Centralblatt f. Bact., 1905, xxxix. 704.
194. MELENEY, H. E., STEARNS, W. W., FORTUINE, S. T., & FERRY, R. M.: “Post-transfusion reactions: a review of 280 transfusions.” Am. Journ. Med. Sci., 1917, cliv. 733.
195. MILLER, G. I.: “Blood transfusion, indications and technique.” Med. Rec., 1915, lxxxviii. 425.
196. MINOT, G. R.: “Methods for testing donors for transfusion of blood and consideration of factors influencing agglutination and hæmolysis.” Boston Med. and Surg. Journ., 1916, clxxiv. 667.
197. MINOT, G. R., & LEE, R. I.: “The blood platelets in hæmophilia.” Arch. Int. Med., 1916, xviii. 474.
[151]
198. MINOT, G. R., & LEE, R. I.: “Treatment of pernicious anæmia, especially by transfusion and splenectomy.” Bost. Med. and Surg. Journ., 1917, clxxvii. 761.
199. MOREL, L.: “Transfusion of blood.” Arch. gen. de Chir., 1914, viii. 1.
200. MOSS, W. L.: “Studies on iso-agglutinins and iso-hemolysins.” Johns Hopkins Hosp. Bull., 1910, xxi. 63.
201. MOSS, W. L.: “Paroxysmal hæmoglobinuria: blood studies in three cases.” Johns Hopkins Hosp. Bull., 1911, xxii. 238.
202. MOSS, W. L.: “A simple method for the indirect transfusion of blood.” Am. Journ. Med. Sci., 1914, cxlvii. 698.
203. MOSS, W. L.: “A simplified method for determining the iso-agglutinin group in the selection of donors for blood transfusion.” Journ. Am. Med. Assoc., 1917, lxviii. 1905.
204. NIX, J. T.: “Blood transfusion simplified. Deductions from nineteen cases, eleven human and eight on dog.” New Orleans Med. and Surg. Journ., 1916, lxix. 435.
205. OEHLECKER, F.: “Bluttransfusion von Vene zu Vene mit Messung der übertragenen Blutmenge.” Zentralbl. f. Chir., 1919, xlvi. 17.
206. OEHLECKER, F.: “Direkte Bluttransfusion von Vene zu Vene bei perniziöse Anæmie.” München. Med. Wchnschr., 1919, lxvi. 895.
207. ORÉ: “Études historiques et physiologiques sur la transfusion du sang.” Paris, 1868.
208. OTTENBERG, R.: “Transfusion and arterial anastomosis.” Ann. Surg., 1908, xlvii. 486.
209. OTTENBERG, R.: “Transfusion and the question of intravascular agglutination.” Journ. of Exp. Med., 1911, xiii. 425.
210. OTTENBERG, R.: “The effect of sodium citrate on blood coagulation in hæmophilia.” Proc. Soc. for Exp. Biol. and Med., 1916, xiii. 104.
211. OTTENBERG, R.: “Medico-legal applications of human blood grouping.” Journ. Am. Med. Assoc., 1921, lxxvii. 682.
212. OTTENBERG, R., & FRIEDMAN, S. S.: “The occur[152]rence of grouped iso-agglutination in the lower animals.” Journ. Exp. Med., 1911, xiii. 531.
213. OTTENBERG, R., & KALISKI, D. J.: “Accidents in transfusion. Their prevention by preliminary examination. Based on an experience of 128 transfusions.” Journ. Am. Med. Assoc., 1913, lxi. 2138.
214. OTTENBERG, R., KALISKI, D. J., & FRIEDMAN, S. S.: “Experimental agglutinative and hemolytic transfusions.” Amer. Journ. Med. Res., 1913, xxviii. 141.
215. OTTENBERG, R., & LIBMAN, E.: “Blood transfusion; indications; results; general management.” Am. Journ. Med. Sci., 1915, cl. 36.
216. OTTENBERG, R., & THALIMER, W.: “Studies in experimental transfusion.” Journ. Med. Res., 1915-16, xxxiii. 213.
217. PANUM, P. L.: “Experimentelle Untersuchungen über die Transfusion, Transplantation, oder Substitution des Blutes in theoretischer und praktischer beziehung.” Virchow’s Arch. f. Path. Anat., 1863, xxvii. 240, 433.
218. PEMBERTON, J. DE J.: “Blood transfusion.” Surg. Gynec. and Obstet., 1919, xxviii. 262. (Also in Collected Papers of the Mayo Clinic, 1918, x. 508.)
219. PEMBERTON, J. DE J.: “Practical considerations of the dangers associated with blood transfusions.” Journ. Iowa State Med. Soc., 1920, x. 170. (Also in Collected Papers of the Mayo Clinic, 1919, xi. 635.)
220. PERCY, N. M.: “A simplified method of blood transfusion, with report of six cases of pernicious anæmia treated by massive blood transfusions and splenectomy.” Surg. Gynec. and Obstet., 1915, xxi. 360.
221. PETERSON, E. W.: “Purpura hæmorrhagica treated by blood transfusion.” Post-Graduate, N.Y., 1914, xxix. 499.
222. PETERSON, E. W.: “Results from blood transfusion in the treatment of severe post-operative anæmia and the hæmorrhagic diseases.” Journ. Am. Med. Assoc., 1916, lxvi. 1291.
223. PÉTREN, G.: “Coagulation time in icterus.” Beitr. z. Klin. Chirurg., 1920, cxx. 501.
[153]
224. PONFICK: “Experimentelle Beiträge zur Lehre von der Transfusion.” Virchow’s Arch. f. Path. Anat., 1875, lxii. 273.
225. POOL, E. H.: “Transfusion and splenectomy for von Jaksch’s anæmia in an infant.” Ann. Surg., March 1915. (In Transact. of N.Y. Surg. Soc.)
226. POOL, E. H., & McCLURE, R. D.: “Transfusion by Carrel’s end-to-end suture method. With report of cases.” Ann. Surg., 1910, lii. 433.
227. POPE, L.: “Simplified transfusion.” Journ. Am. Med. Assoc., 1913, lx. 1284.
228. PRIMROSE, A.: “The value of the transfusion of blood in the treatment of the wounded in war.” Ann. Surg., 1918, lxviii. 118.
229. PRIMROSE, A., & RYERSON, E. S.: “The direct transfusion of blood, its value in hæmorrhage and shock and in treatment of the wounded in the war.” Brit. Med. Journ., 1916, ii. 384.
230. RAMIREZ, M. A.: “Horse asthma following blood transfusion.” Journ. Am. Med. Assoc., 1919, lxxiii. 984.
231. RAMSAY, J.: “Transfusion of blood in nephritis.” Brit. Med. Journ., 1920, i. 766.
232. RANSOM, S. H.: “The treatment of staphylococcus septicæmia by transfusion of immune blood.” Ann. Surg., 1917, lxvi. 513.
233. RAULSTON, B. O., & WOODYATT, R. T.: “Blood transfusion in diabetes mellitus.” Journ. Am. Med. Assoc., 1914, lxii. 996.
234. RICHARDSON, B. W.: “The cause of coagulation of the blood. The Astley Cooper prize essay for 1856, with additional observations and experiments.” London, 1858.
235. RICHARDSON, E. H.: “Treatment of the emergency cases of ectopic pregnancy.” Johns Hopkins Hosp. Bull., 1916, xxvii. 262.
236. ROBERTSON, L. B.: “The transfusion of whole blood.” Brit. Med. Journ., 1916, ii. 38.
237. ROBERTSON, L. B.: “A contribution on blood transfusion in war surgery.” Lancet, 1918, i. 759.
[154]
238. ROBERTSON, L. B.: “Blood transfusion in hæmorrhagic disease of the new-born.” Brit. Med. Journ., 1921, i.
239. ROBERTSON, L. B.: “Blood transfusion in severe burns in infants and young children.” Canad. Med. Assoc. Journ., 1921, xi. 744.
240. ROBERTSON, L. B., & WATSON, C. G.: “Further observations on the results of blood transfusion in war surgery.” Ann. Surg., 1918, lxvii. 1.
241. ROBERTSON, O. H.: “The effects of experimental plethora on blood production.” Journ. Exper. Med., 1917, xxvi. 221.
242. ROBERTSON, O. H.: “A method of citrated blood transfusion.” Brit. Med. Journ., 1918, i. 477.
243. ROBERTSON, O. H.: “Transfusion with preserved red cells.” Brit. Med. Journ., 1918, i. 691.
244. ROBERTSON, O. H.: “Memorandum on blood transfusion.” Rep. of the Med. Res. Com., iv. 1919, 143.
245. ROBERTSON, O. H., & BOCK, A. V.: “Memorandum on blood volume after hæmorrhage.” Rep. of the Med. Res. Com., vi. 1919, 213.
246. ROBERTSON, O. H., & BOCK, A. V.: “Blood volume in wounded soldiers.” Journ. Exp. Med., 1919, xxix. 139.
247. ROSE, A.: “A case of melæna neonatorum successfully treated by the injection of blood serum.” Brit. Med. Journ., 1917, ii. 762.
248. ROSE, C. W., & HUND, E. J.: “Treatment of pneumonic disturbances complicating influenza.” Journ. Am. Med. Assoc., 1919, lxxii. 642.
249. ROUS, P., & TURNER, J. R.: “The preservation of living red blood cells in vitro. I. Methods of preservation. II. The transfusion of kept cells.” Journ. Exp. Med., 1916, xxiii. 219.
250. ROUS, P., & WILSON, G. W.: “Fluid substitutes for transfusion after hæmorrhage.” Journ. Am. Med. Assoc., lxx. 219-222.
251. RUECK, G. A.: “Transfusion by the gravitation method.” Med. Rec., 1915, lxxxvii. 354.
252. SALANT, W., & WISE, L. E.: “The action of sodium citrate and its decomposition in the body.” Journ. Biolog. Chem., 1917, xxviii. 27.
[155]
253. SANFORD, A. H.: “Iso-agglutination groups: a diagram showing their interrelation.” Journ. Am. Med. Assoc., 1916, lxvii. 808.
254. SANFORD, A. H.: “Selection of the donor for transfusion.” Journ. Lancet, 1917, xxxvii. 698.
255. SANFORD, A. H.: “A modification of the Moss method of determining iso-hæmagglutination groups.” Journ. Am. Med. Assoc., 1918, lxx. 1221. (Also in Collected Papers of the Mayo Clinic, 1918, x. 504.)
256. SATTERLEE, H. S., & HOOKER, R. S.: “Experiments to develop a more widely useful method of blood transfusion.” Arch. Int. Med., 1914, xiii. 51.
257. SATTERLEE, H. S., & HOOKER, R. S.: “The further development of an apparatus for the transfusion of blood.” Surg. Gynec. and Obst., 1914, xix. 235.
258. SATTERLEE, H. S., & HOOKER, R. S.: “The use of hirudin in the transfusion of blood.” Journ. Am. Med. Assoc., 1914, lxii. 1781.
259. SATTERLEE, H. S., & HOOKER, R. S.: “Transfusion of blood, with special reference to the use of anticoagulants.” Journ. Am. Med. Assoc., 1916, lxvi. 618.
260. SAUERBRUCH: “Artery of donor introduced directly into recipient’s vein for transfusion of blood.” Münch. Medizin. Wchnschr., 1915, lxii. No. 45.
261. SCHEEL, O., & BANG, O.: “Transfusion in a case of pernicious anæmia.” Norsk Mag. f. Lægevidenskaben, 1920, March.
262. SCHLOSS, C. M., & COMMINSKEY, L. J. J.: “Spontaneous hæmorrhage in the new-born.” Am. Journ. Dis. Child., 1911, i. 276.
263. SCHULTZ, W.: In Gravitz. “Klinische Pathologie des Blutes.” Leipsic, 1911, p. 381.
264. SCHWEITZER: “Blood reinfusion in extra-uterine pregnancy.” Münch. Med. Wchnschr., 1921, lxviii. 699.
265. SIMONS, I.: “Experiences with the sodium citrate method of indirect transfusion of blood.” Journ. Am. Med. Assoc., 1915, lxv. 1339.
266. SHATTOCK, S. G.: “Chromocyte clumping in acute pneumonia and certain other diseases, and the signific[156]ance of the buffy coat in the shed blood.” Journ. Path. and Bact., 1900, vi. 303.
267. SMITH, T.: “Transfusion of blood in the case of a patient suffering from purpura.” Lancet, 1873, i. 837.
268. SORESI, A. L.: “New instrument for direct transfusion of blood and temporary anastomosis between blood vessels.” XVI. Internat. Med. Congr., Budapest, 1909.
269. SORESI, A. L.: “Clinical indications for direct transfusion of blood, with the author’s technique.” Med. Rec., 1912, lxxxi. 835.
270. SPENCER, W. G.: “Transfusion of blood in civil practice.” Med. Sci. Abstr. and Rev., 1919, i. 309.
271. STANLEY, L. L.: “Blood transfusion apparatus.” Journ. Am. Med. Assoc., 1920, lxxiv. 671.
272. STANSFELD, A. E.: “The principles of the transfusion of blood.” Lancet, 1917, i. 488.
273. STANSFELD, A. E.: “An apparatus for the transfusion of blood by the citrate method.” Lancet, 1918, i. 334.
274. SYDENSTRICKER, V. P. W., MASON, V. R., & RIVERS, T. M.: “Transfusion of blood by the citrate method.” Journ. Am. Med. Assoc., 1917, lxviii. 1677.
275. TARR, E. M.: “Intravenous injections in infancy. Advantage of the superior longitudinal sinus route.” Arch. Pediatr., 1919, xxxvi. 71.
276. TELFER, S. V.: “Note on the preparation of sterile gum acacia solution for intravenous injection.” Rep. of the Med. Res. Com., i., 1919, 42.
277. TERRIEN, E.: “Transfusion of blood in malignant measles.” Bull. Soc. Méd. des Hôp., 1919, xliii. 1134.
278. THALIMER, W.: “Hæmoglobinuria after a second transfusion with the same donor.” Journ. Am. Med. Assoc., 1921, lxxvi. 1345.
279. THOMAS, T. G.: “The intravenous injection of milk as a substitute for the transfusion of blood.” N.Y. Med. Journ., 1878, xxvii. 449.
280. UNGER, L.: “Melæna neonatorum.” Wien. Klin. Woch., 1912, xxxix.
281. UNGER, L. J.: “A new method of syringe transfusion.” Journ. Am. Med. Assoc., 1915, lxiv. 582.
282. UNGER, L. J.: “Recent simplifications of the syringe[157] method of transfusion.” Journ. Am. Med. Assoc., 1915, lxv. 1029.
283. UNGER, L. J.: “Transfusion of unmodified blood, an analysis of one hundred and sixty-five cases.” Journ. Am. Med. Assoc., 1917, lxix. 2159.
284. UNGER, L. J.: “Precautions necessary in the selection of a donor for blood transfusion.” Journ. Am. Med. Assoc., 1921, lxxvi. 9.
285. VINCENT, B.: “Blood transfusion for hæmorrhagic diseases of the new-born. The use of the external jugular vein in infants.” Boston Med. and Surg. Journ., 1912, clxvi. 627.
286. VINCENT, B.: “Blood transfusion with paraffin-coated needles and tubes.” Surg. Gynec. and Obstet., Nov. 1916.
287. VINES, H. W. C.: “Anaphylaxis in the treatment of hæmophilia.” Quart. Journ. Med., 1920, xiii. 257.
288. VINES, H. W. C.: “The coagulation of the blood. I. The rôle of calcium. II. The clotting complex.” Journ. Phys., 1921, lv. 86, 287.
289. VOGEL, K. M., & McCURDY, U. F.: “Blood transfusion and regeneration in pernicious anæmia.” Arch. Internal. Med., 1913, xii. 707.
290. WAAG, A.: “Repeated small injections of blood in pernicious anæmia.” Münch. Medizin. Wchnschr., 1921, lxviii. 677.
291. WALLICH, V., & LEVADITI, C.: “Recherches sur les réactions sanguines, à considérer à propos de la transfusion de sang.” Bull. de l’Acad. de Méd., 1914, lxxviii. No. 17.
292. WARD, G.: “Transfusion of plasma.” Brit. Med. Journ., 1918, i. 301.
293. WATSON, J. J.: “A method of fixation of vein to facilitate the introduction of a needle for intravenous injections.” Journ. Am. Med. Assoc., 1911, lvii. 383.
294. WAUGH, W. G.: “An investigation of the end result in one hundred and twenty-four cases of blood transfusion.” Brit. Med. Journ., 1919, ii. 39.
295. WEIL, P. E.: “Serum treatment of hæmophilia.” Lancet, 1920, ii. 300.
[158]
296. WEIL, R. J.: “Sodium citrate in the transfusion of blood.” Journ. Am. Med. Assoc., 1915, lxiv. 425.
297. WILLIAMSON, H.: “Blood transfusion before operation in severe secondary anæmias.” Lancet, 1920, i. 867.
298. WOLTMANN, H.: “Transfusion by the citrate method in a sixty-hour-old baby with melæna neonatorum.” Am. Journ. Med. Sci., 1915, lxv. 2163.
299. WREN, SIR C.: “An account of the rise and attempts of a way to conveigh liquors immediately into the mass of blood.” Philosophical Trans., 1665, i. 128.
300. ZIEMSSEN, VON: “Ueber die subcutane Blutinjection und über eine einfache Methode der intravenösen Transfusion.” Münch. Med. Wchnschr., 1892, xix. 323.
301. ZIMMERMANN, R.: “Blood transfusion in gynæcological cases.” Münch. Med. Wchnschr., 1920, lxvii. 898.
302. ZIMMERMANN, R.: “Testing donor’s blood before transfusion.” Zentralbl. f. Chir., Leipzig, 1920, xliv. 1146.
[159]
[1] The first reference to this that I can find is in “Moines et Papes,” by Emile Gebhardt, La Chronique Médicale, November 1912.
[2] Life and Times of Rodrigo Borgia, A. H. Mathew, D.D., 1912, p. 66.
[3] This refers to the experiment of Denys, mentioned above.
[4] Birch’s History of the Royal Society, 1756, ii. p. 216.
[5] The notation used here is that initiated by Moss in 1910. This does not agree with the notation introduced three years previously by Jansky, the Groups I and II of Moss corresponding to the Groups IV and III of Jansky and vice versa. The difference has given rise to confusion and some disasters, and it has been recently recommended by an American Medical Committee that the notation of Jansky be universally adopted on grounds of priority. This decision is no doubt fully justified in American practice, but in this country the notation of Moss has been so generally used that I have not attempted to reverse it. The possible dangers that may arise should, however, be realized.
[6] Mendelism, R. C. Punnett, 5th ed., Macmillan, 1919.
[7] J. A. Kolmer, Infection, Immunity, and Specific Therapy, ed. 2, Saunders Co., 1917, p. 287: “With the increasing number of blood transfusions the phenomena of iso-agglutination and iso-hæmolysis are of considerable practical importance, especially if the patient is suffering from cancer, when the serum is likely to be actively hæmolytic for the donor’s corpuscles.” No authority is given.
[8] This embodies the same principle as the “dropper” designed by R. D. Laurie.
[9] A very convenient form of tourniquet is that designed by R. G. Canti. It is sold by Messrs. Maw & Sons, and by Messrs. Allen & Hanburys.